Introduction
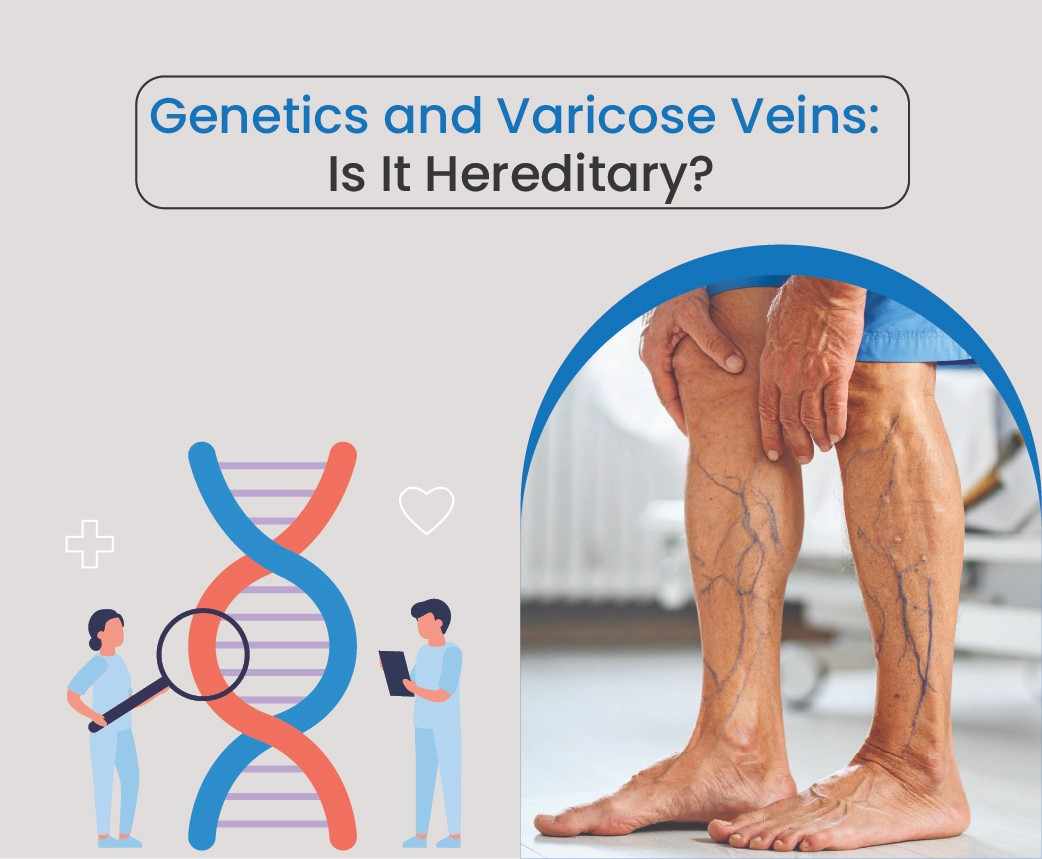
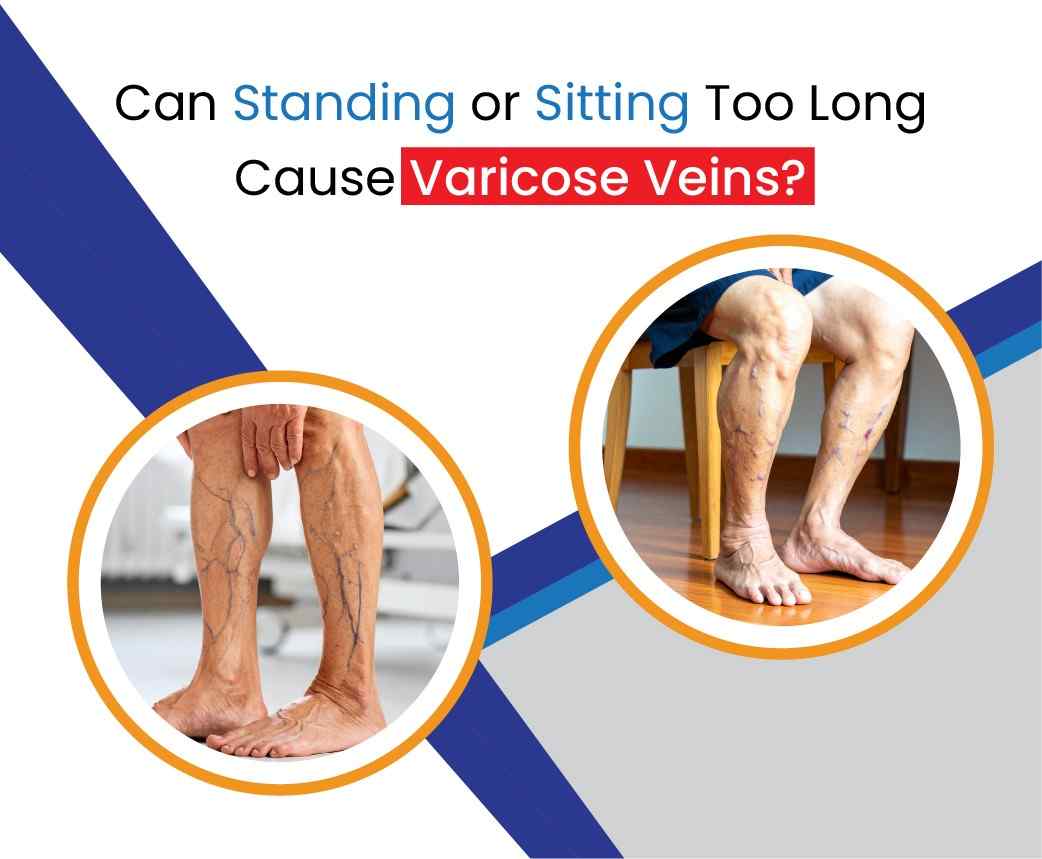
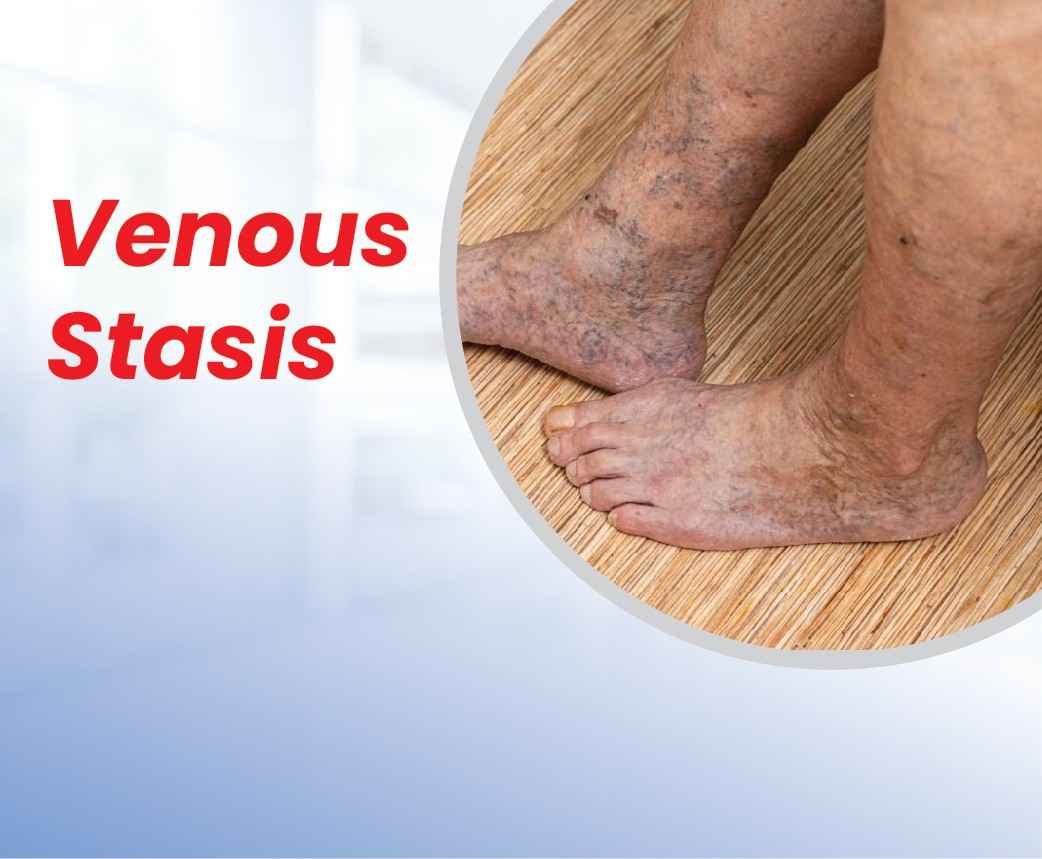
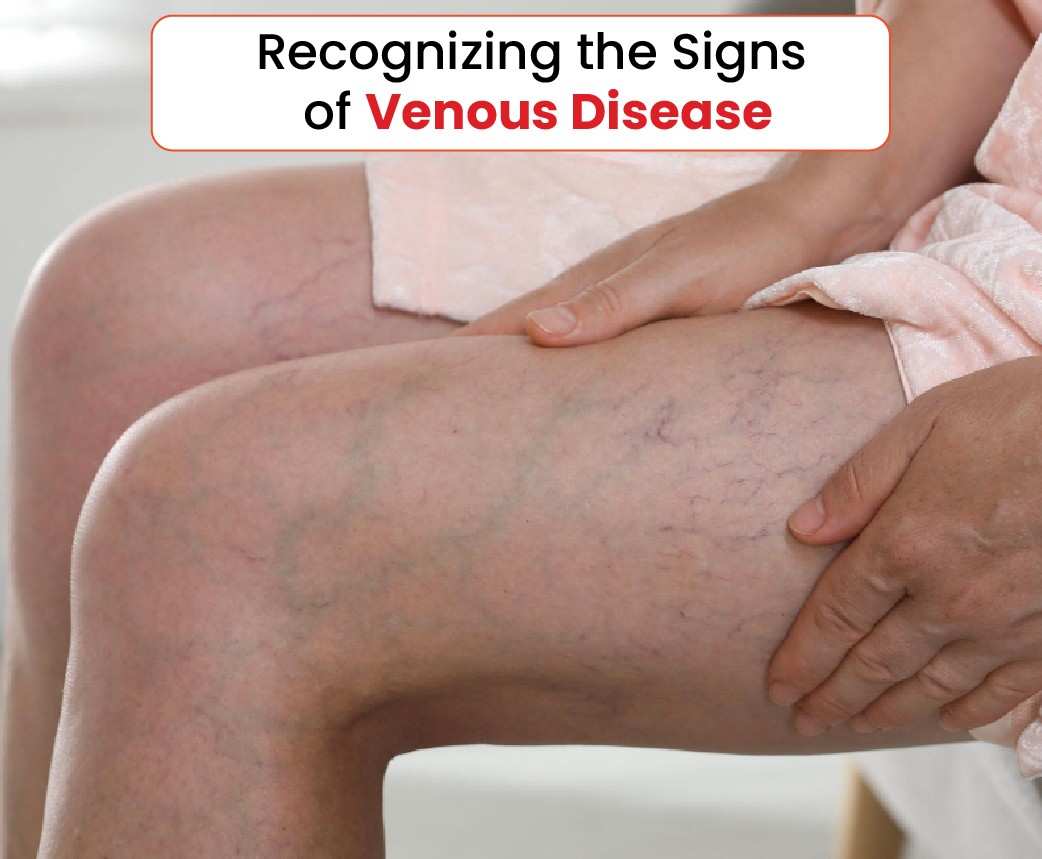
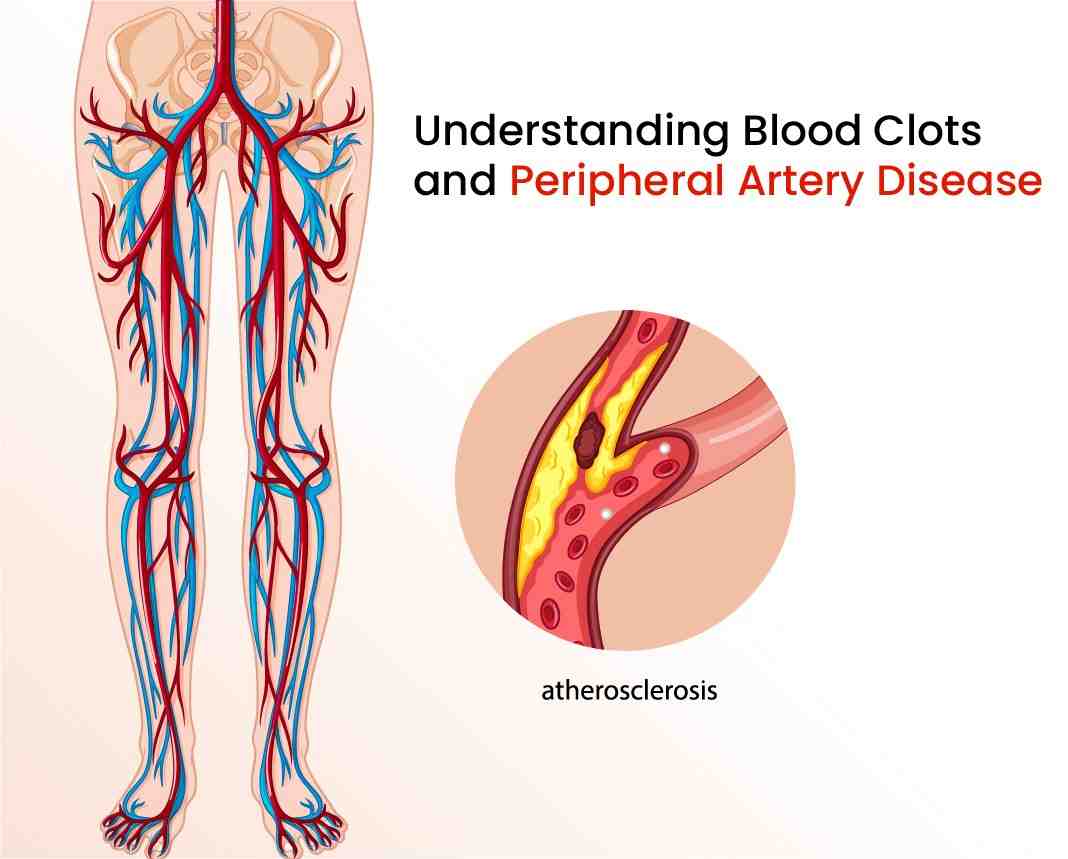
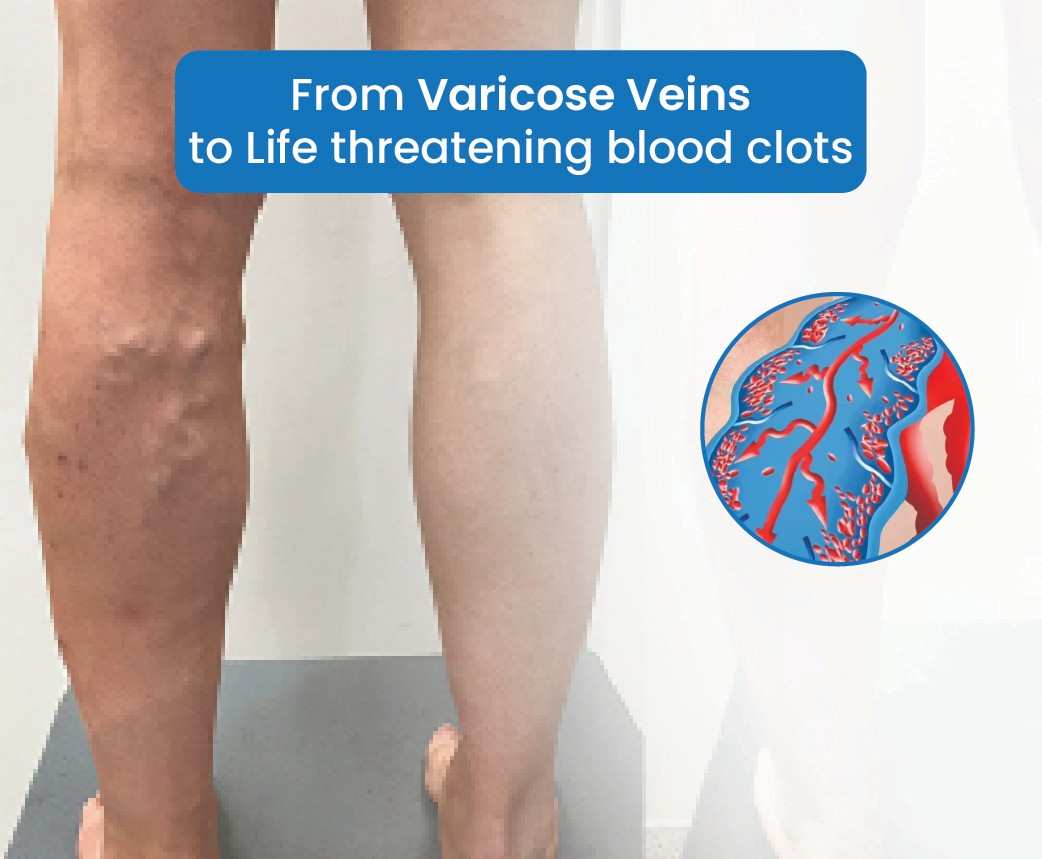
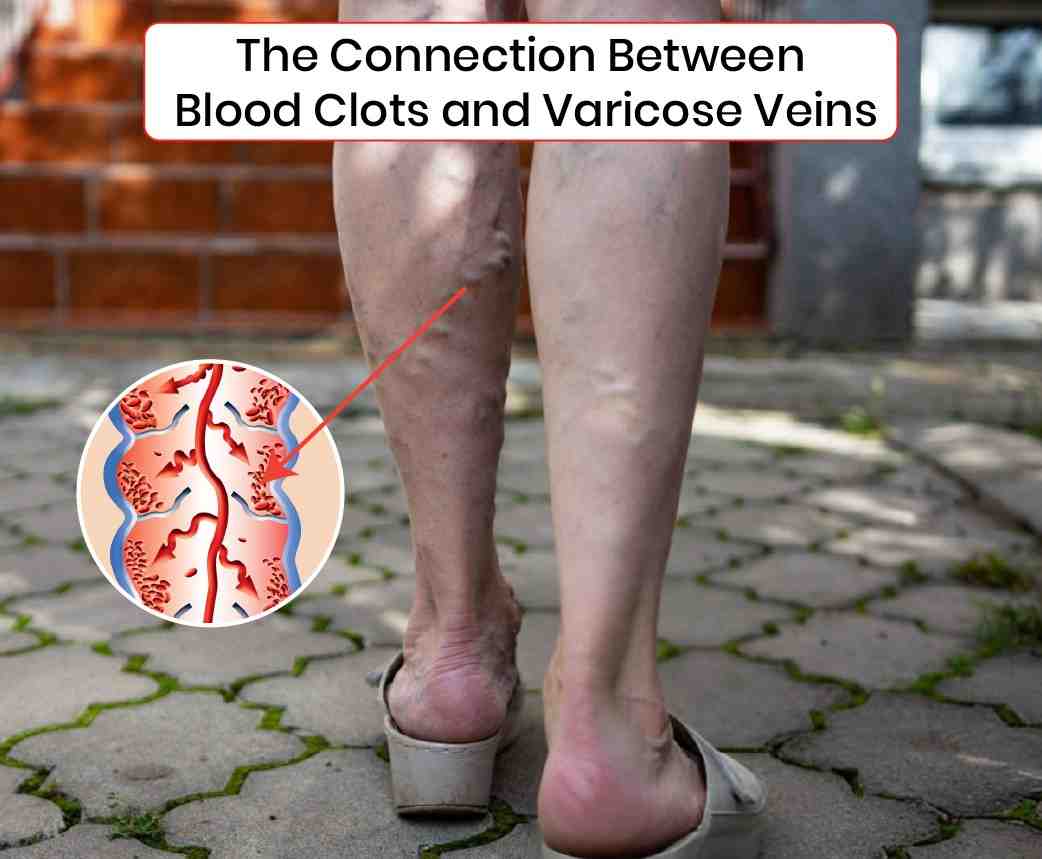
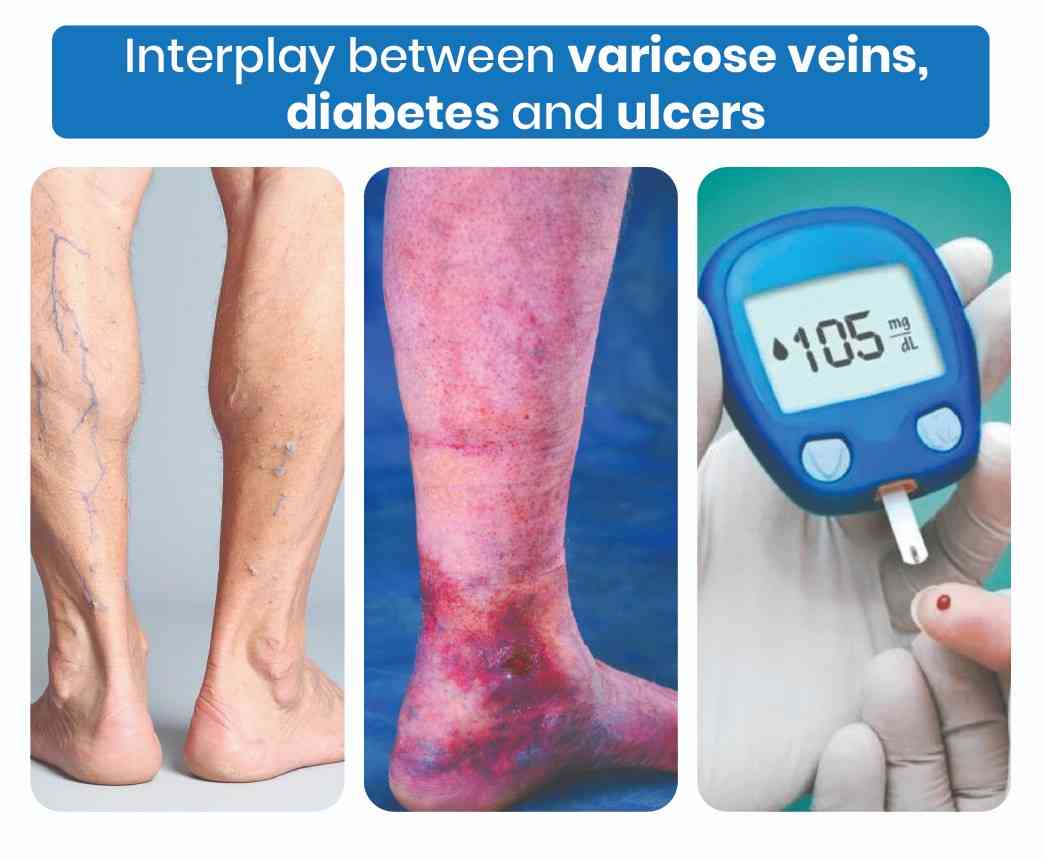
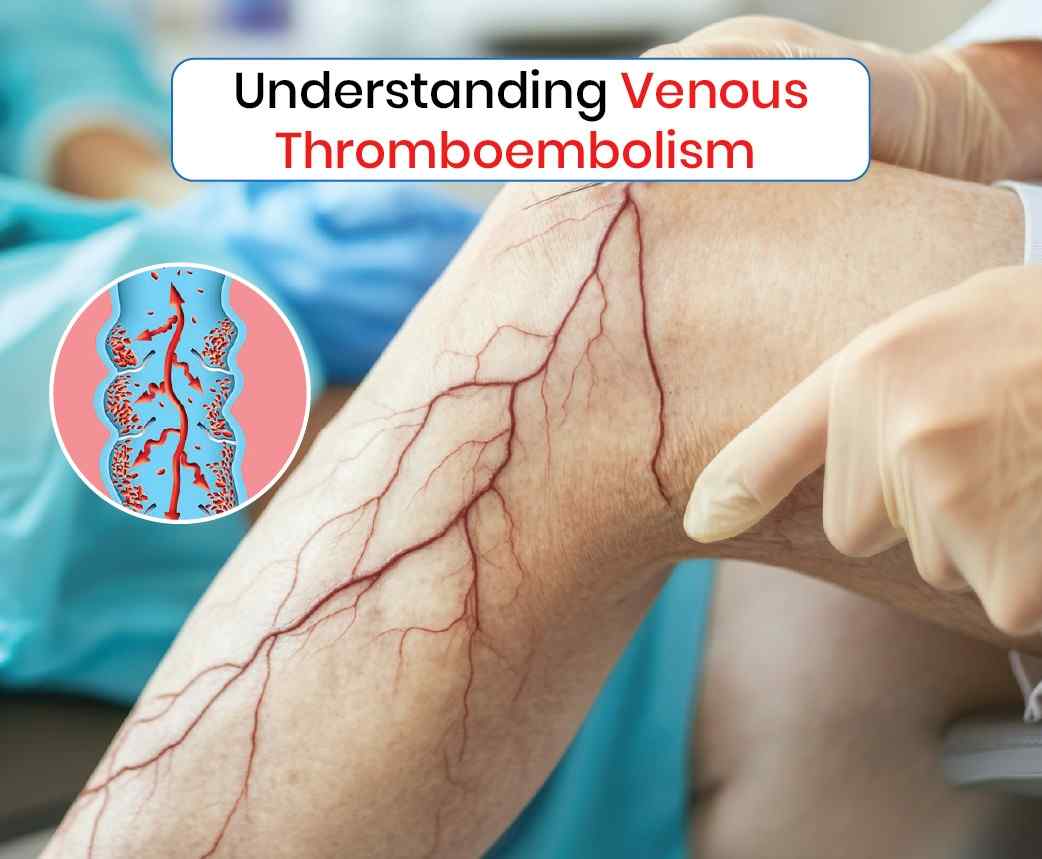
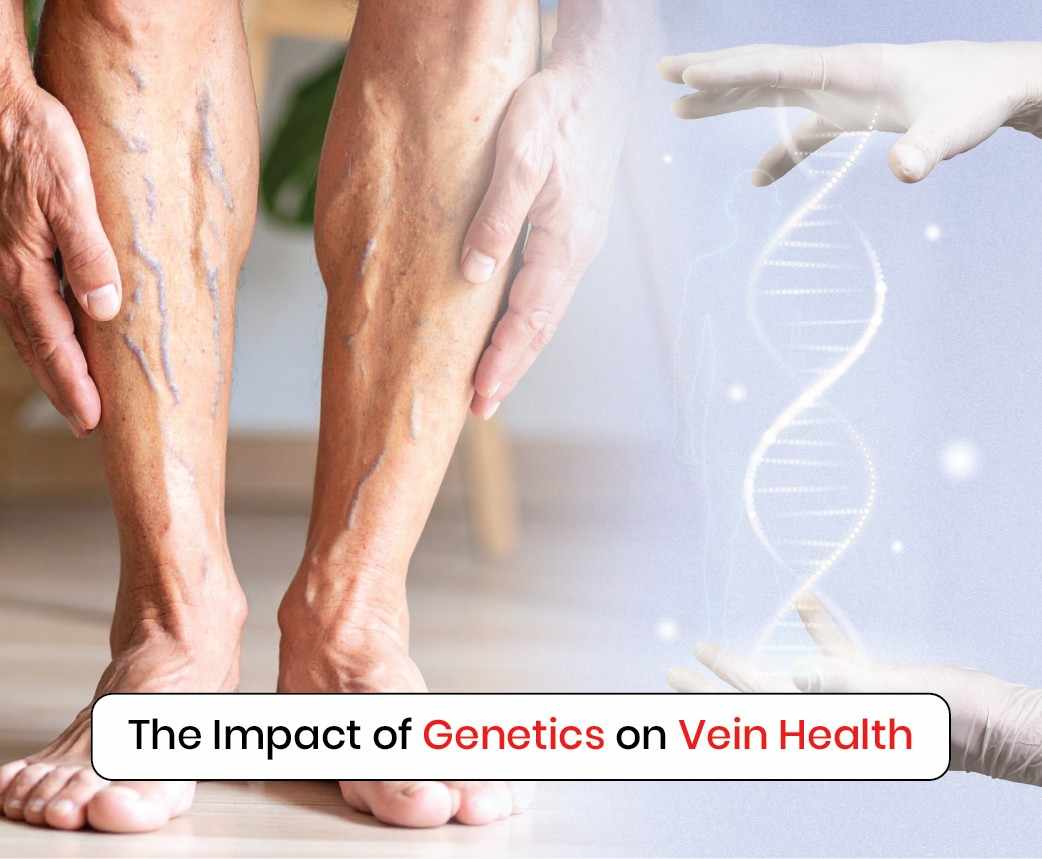
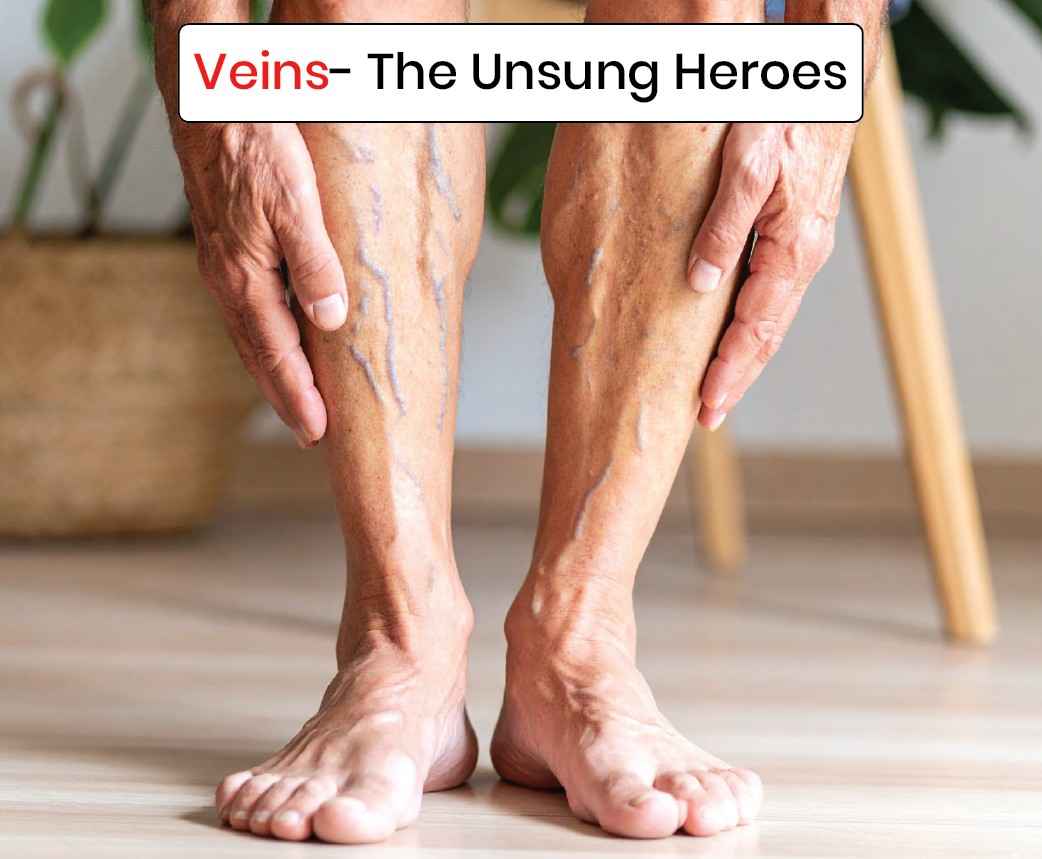
Varicose veins are not just a cosmetic problem; they are a vascular condition that can cause leg pain, swelling, heaviness, skin discoloration, and even ulcers if left untreated. In Hyderabad, where lifestyle and long working hours often worsen vein issues, patients are increasingly looking for modern, painless solutions. Avis Vascular Centre has emerged as the No. 1 varicose veins hospital in Hyderabad, known for its advanced technology, globally trained specialists, and patient-focused care.
Why Avis Vascular Centre?
At the core of Avis Hospitals’ success is Dr. Rajah V. Koppala, an internationally trained interventional radiologist. His expertise in minimally invasive vascular treatments has brought global best practices to Hyderabad. With branches in Jubilee Hills and Kukatpally, Avis is easily accessible for patients across the city.
Avis focuses exclusively on vascular and interventional radiology, which means patients get the benefit of highly specialised care that goes beyond general surgery.
Advanced Varicose Vein Treatments at Avis
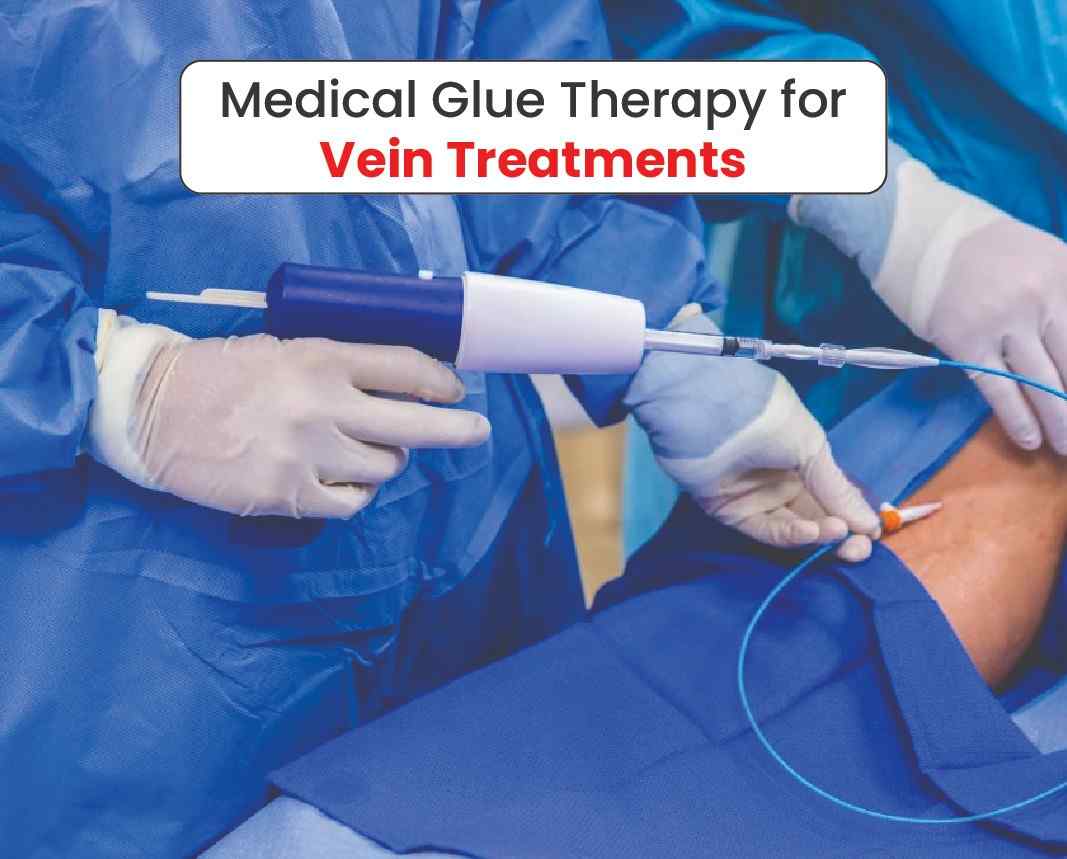
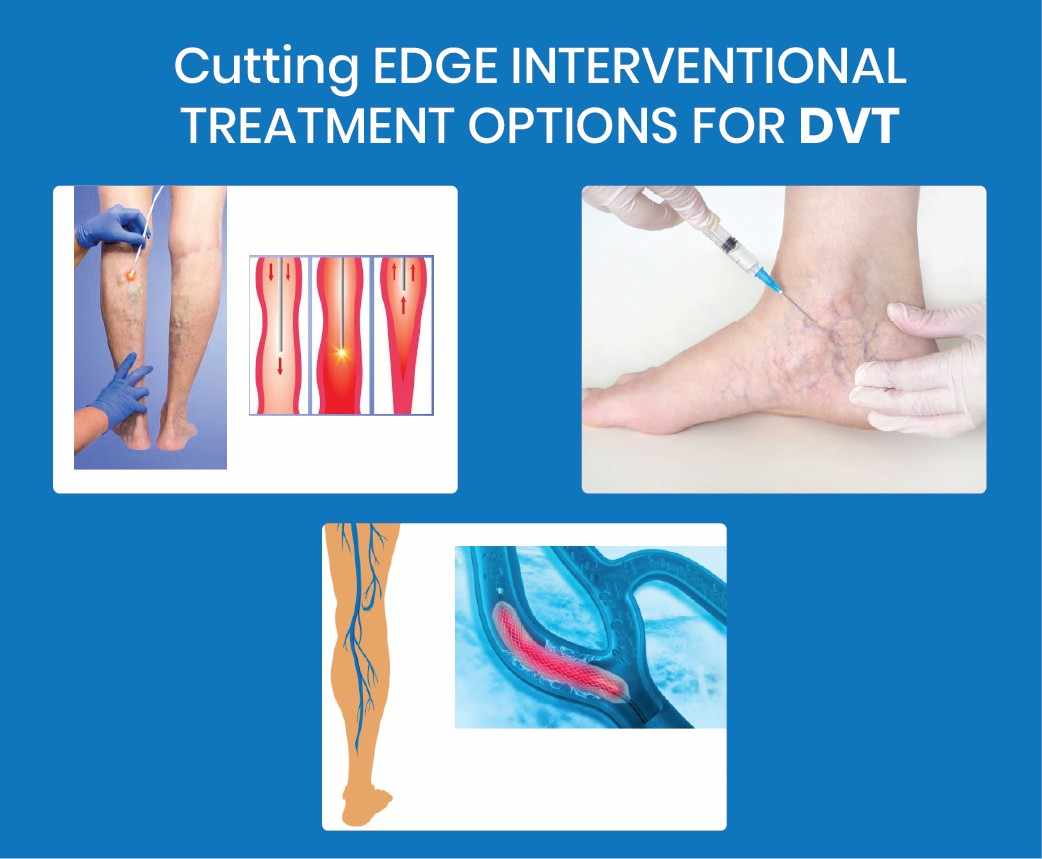
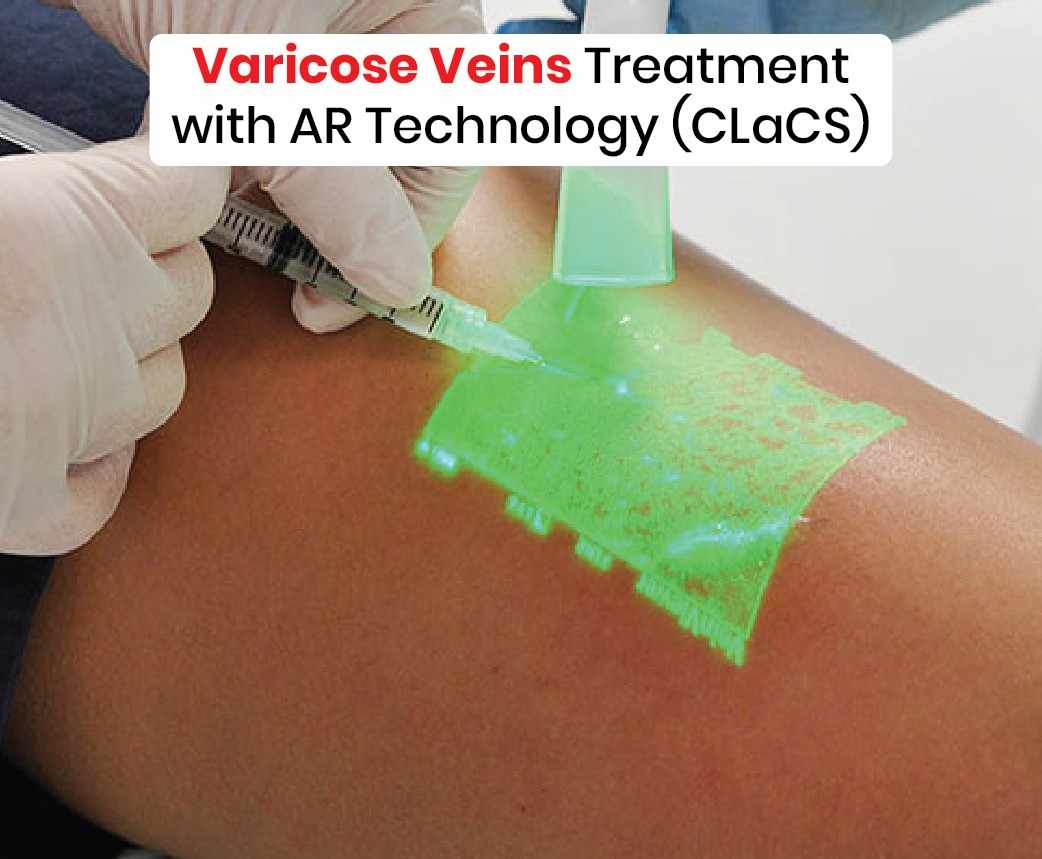
One of the key reasons patients rate Avis as the best for varicose veins treatment in Hyderabad is its cutting-edge, minimally invasive procedures.
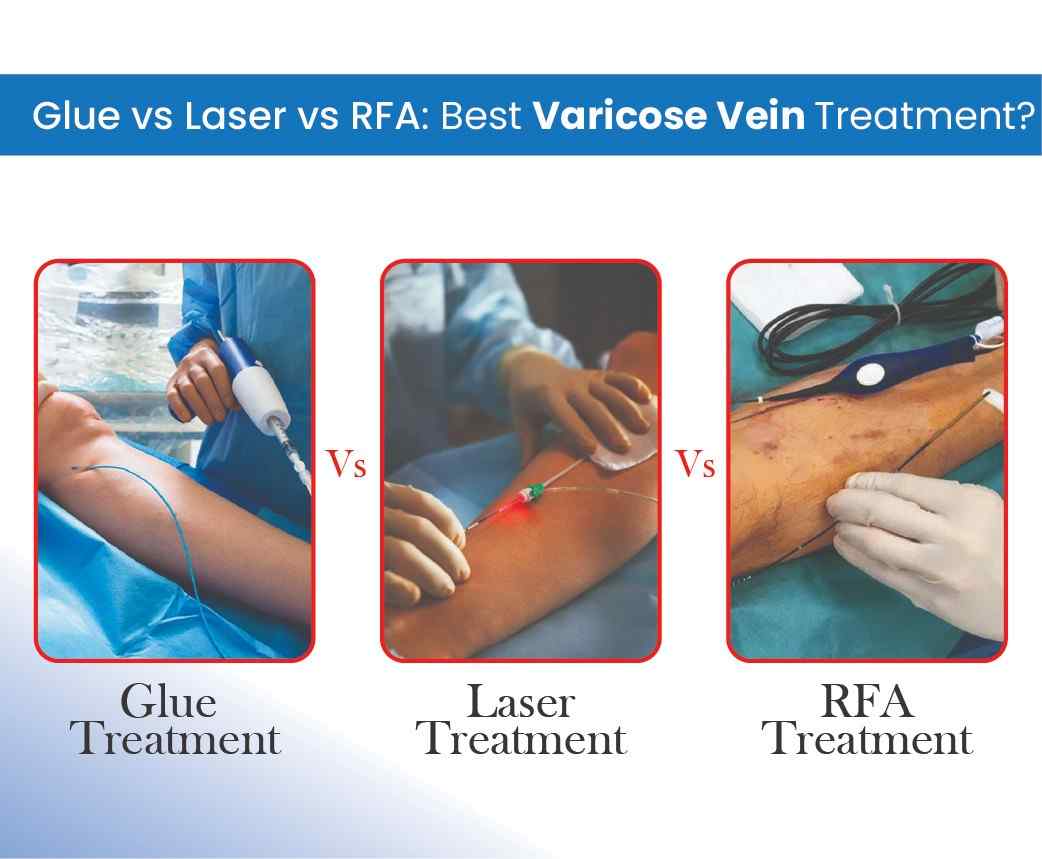
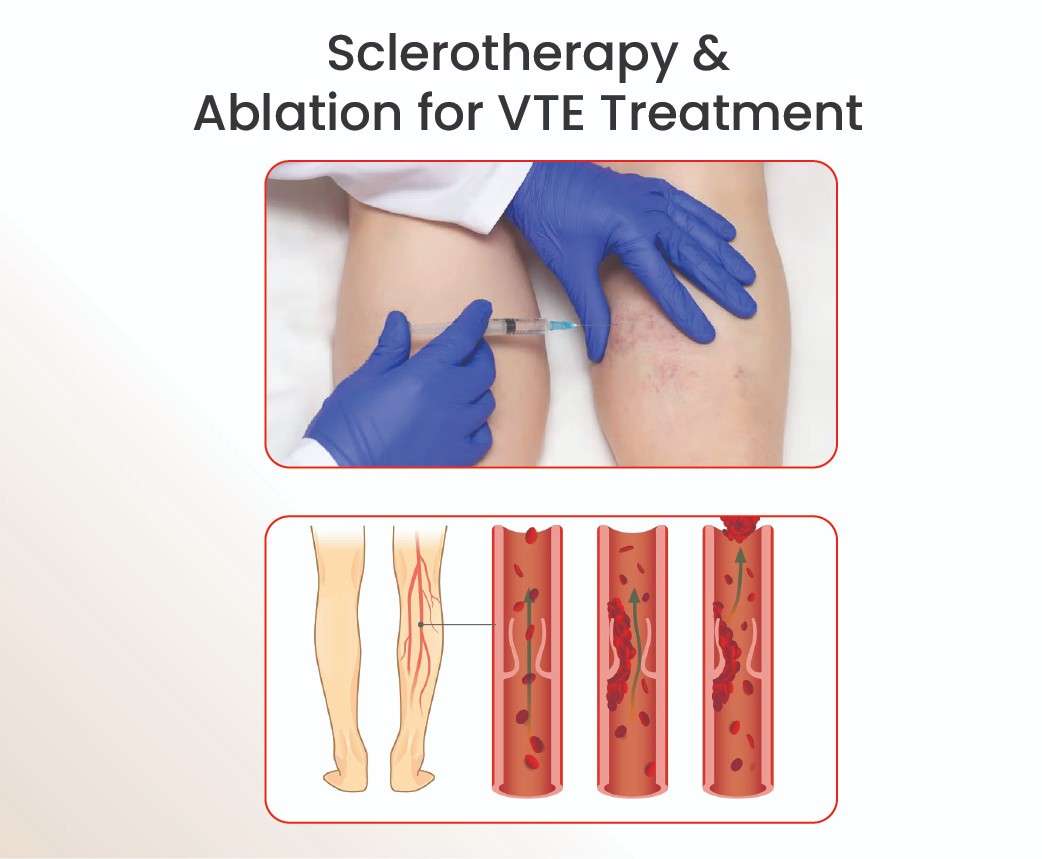
– Endovenous Laser Ablation (EVLA): A laser-based treatment to seal damaged veins.
– Radiofrequency Ablation (RFA): Heat energy closes faulty veins with precision.
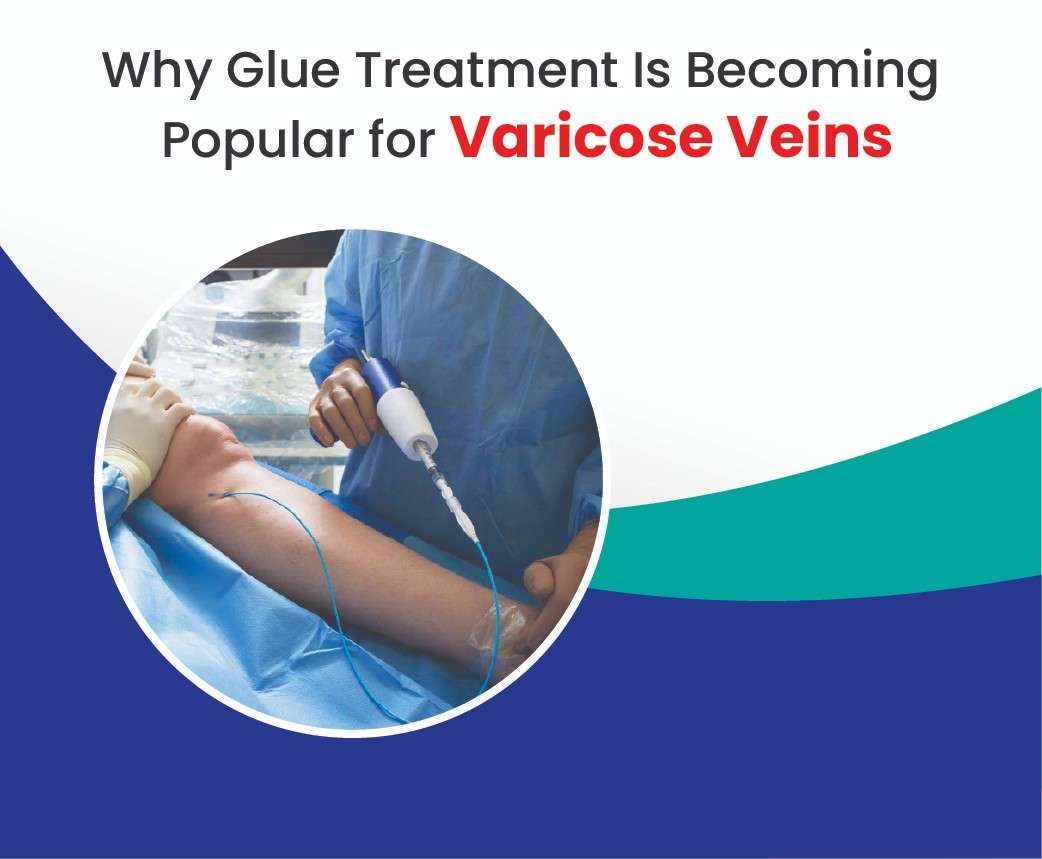
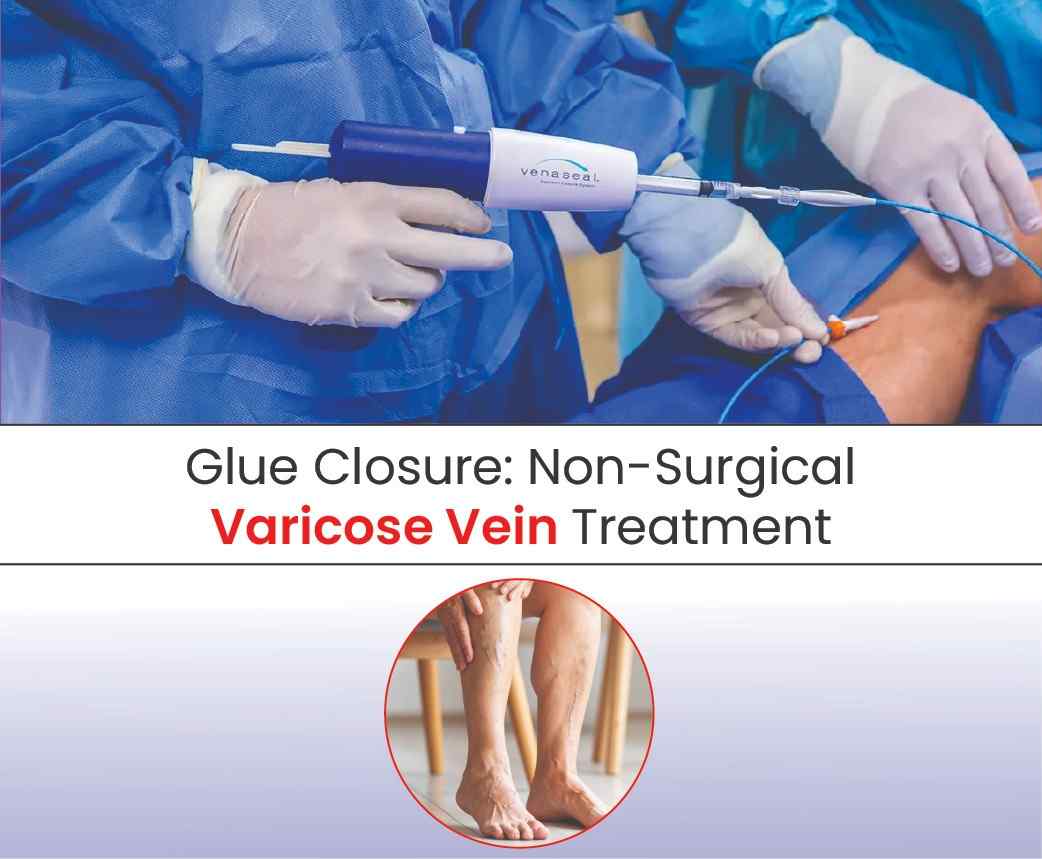
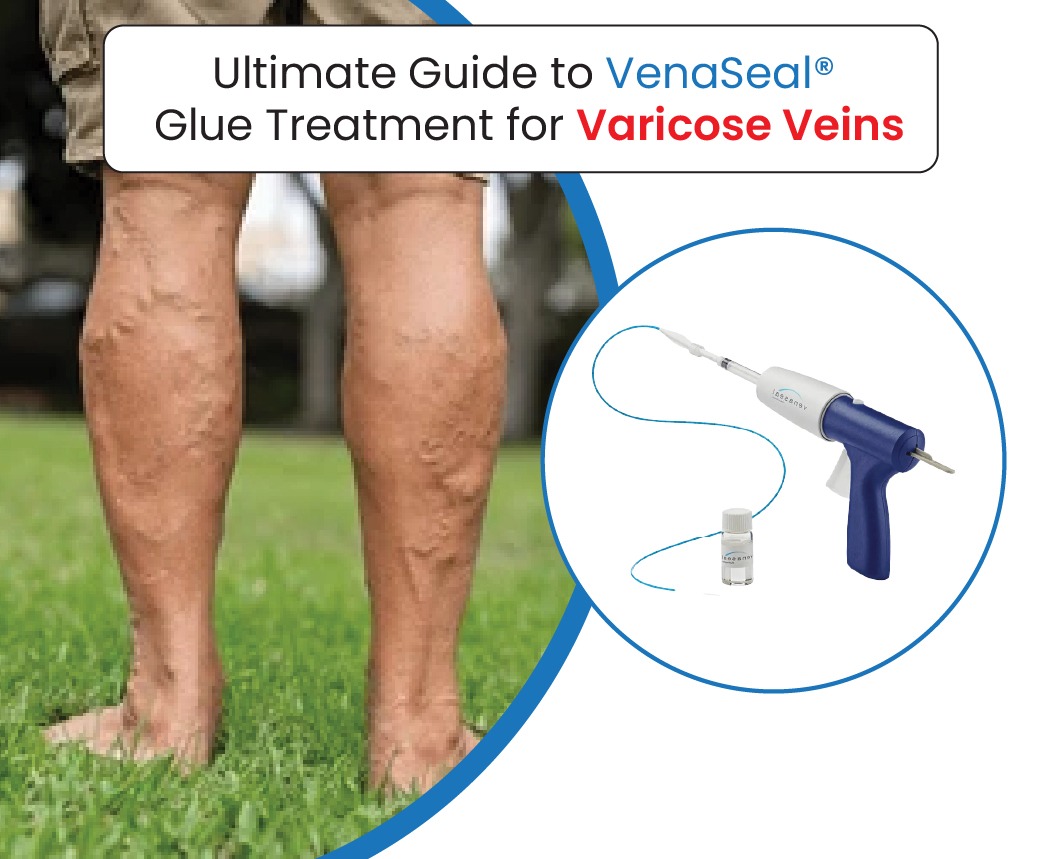
– Vein Glue Closure (Cyanoacrylate Adhesive): A painless, stitch-free solution.
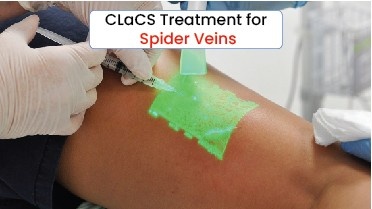
– CLaCS (Cryo + Laser + Cryo Sclerotherapy): Highly effective for spider veins.
– Ulcer Management & Skin Grafting: For advanced venous disease and complications.
All procedures are:
– Day-care based (no hospital stay required)
– Performed under local anaesthesia
– Painless, scar-free, and with quick recovery times
Patient-Centric Care
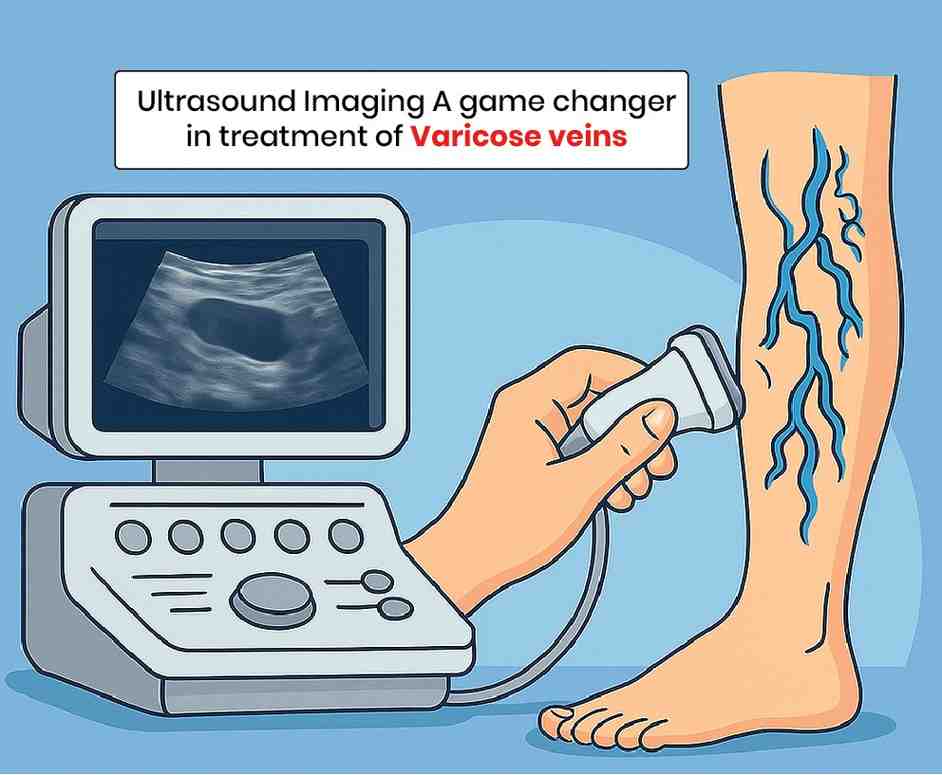
At Avis, patients are not treated with a one-size-fits-all approach. Each case begins with a free Doppler ultrasound screening (worth ₹4,500) to map the venous system and identify the exact problem. The hospital ensures:
– Customised treatment plans
– Insurance and transparent pricing
– Regular follow-up appointments
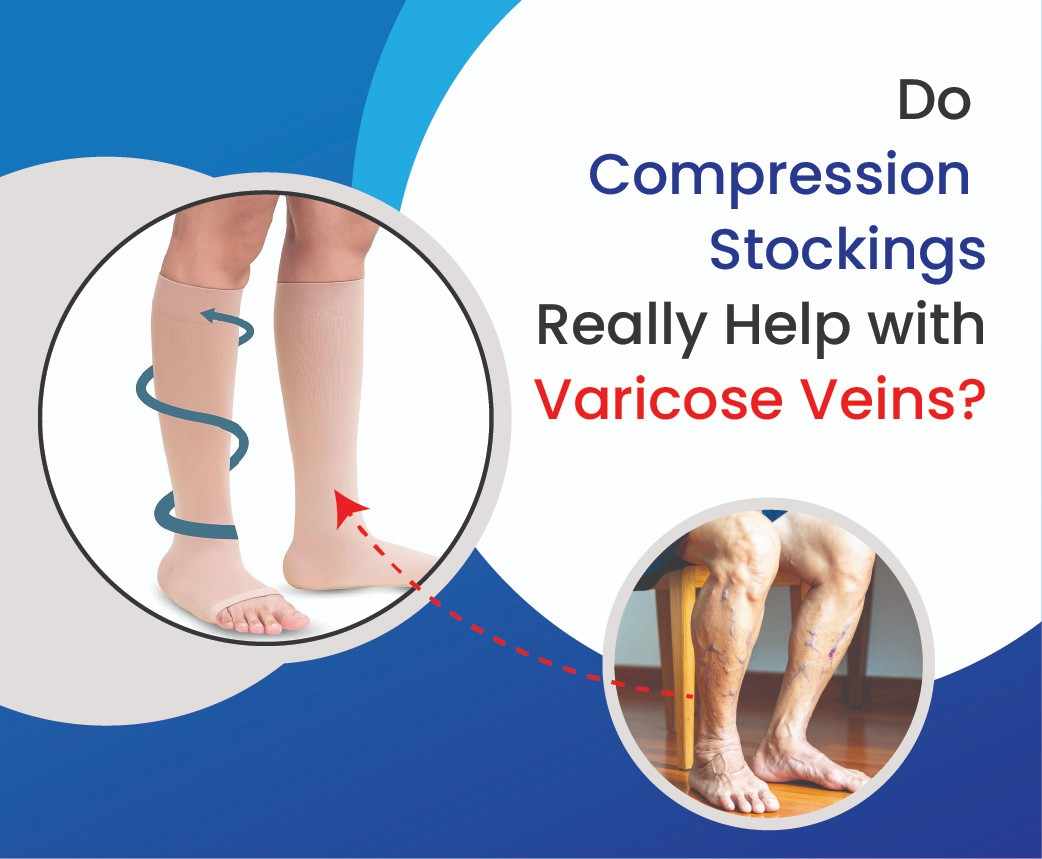
– Guidance on lifestyle changes such as exercise, compression stockings, and diet to prevent recurrence
Why Avis is the No. 1 Choice
– Globally trained vascular experts
– USFDA-approved technologies
– Thousands of successful procedures in Hyderabad
– Patient reviews praising comfort, care, and fast results
– Convenient locations in prime areas of the city
When to See a Specialist
Visit Avis Hospitals if you notice:
– Persistent heaviness or leg pain
– Bulging or twisted veins
– Swelling, itching, or skin discoloration
– Non-healing ulcers
– Restless legs or night cramps
Early consultation ensures faster recovery and prevents complications.
For patients in Hyderabad, Avis Vascular Centre is more than just a treatment centre it is a trusted partner in restoring leg health and confidence. By combining global expertise, advanced laser-based technologies, and patient-first care, Avis truly stands as the No. 1 varicose veins hospital in Hyderabad.
If you are struggling with varicose or spider veins, Avis Vascualr Centre offers safe, effective, and lasting solutions that put your comfort and health first.