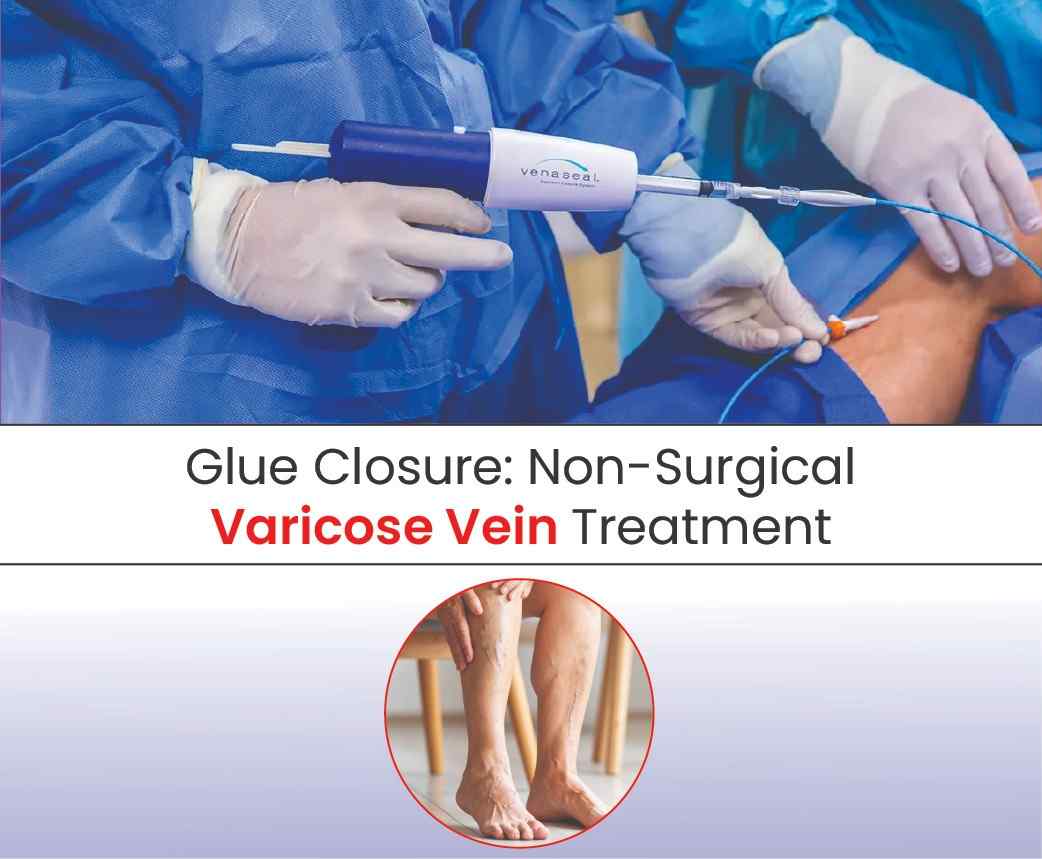
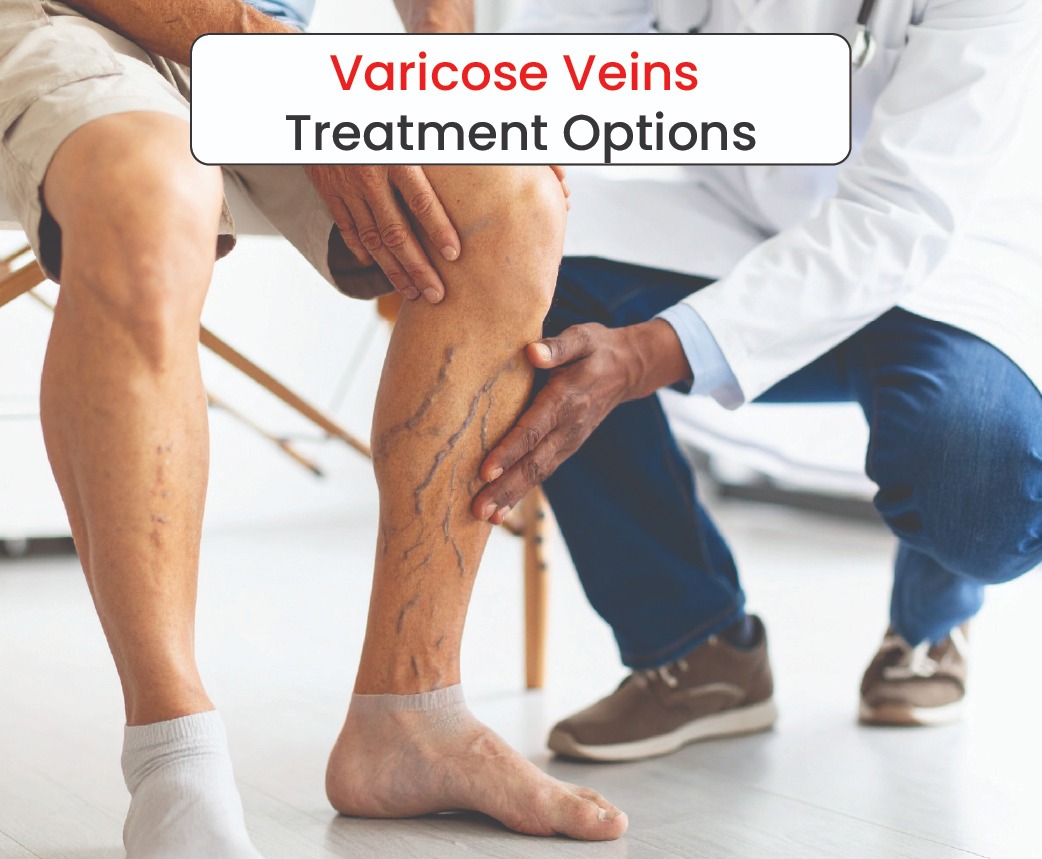
For working professionals, time is often the most valuable commodity. Long hours at a desk, standing on the shop floor, or travelling for business can make varicose veins worse — causing heaviness, swelling, discomfort, and visible bulging veins. Left untreated, they can also lead to skin changes, ulcers, or clots.
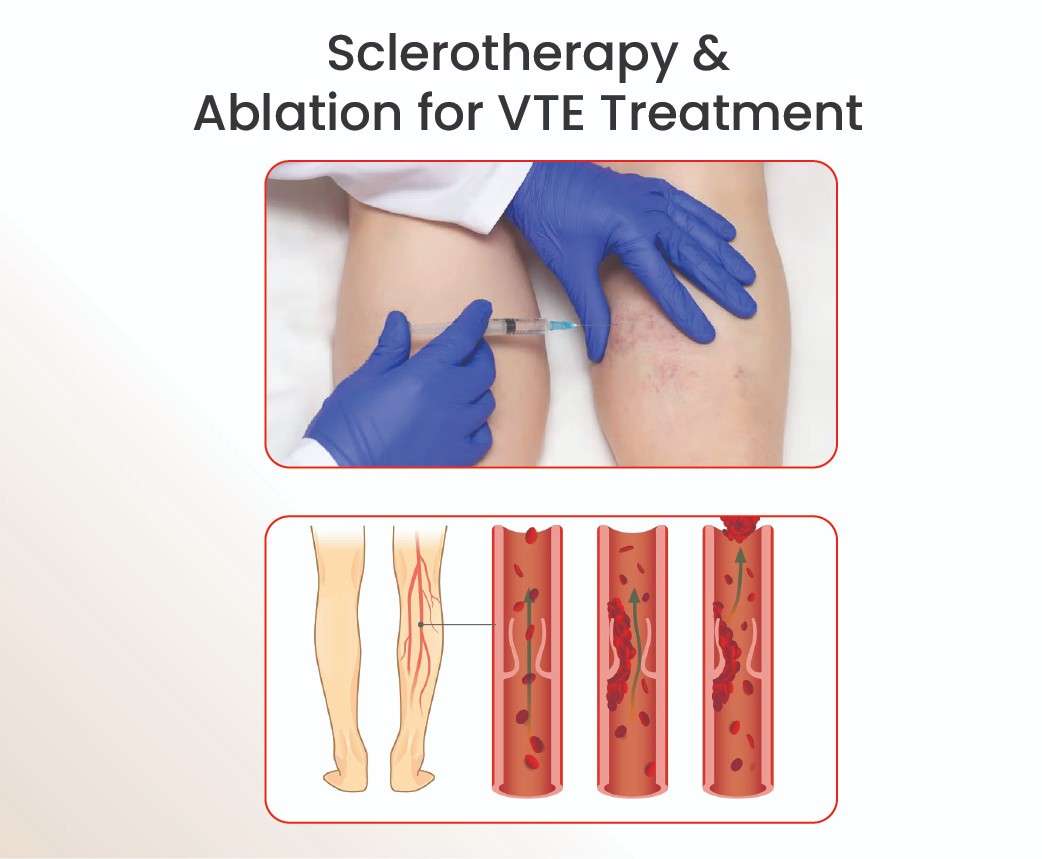
While traditional surgical and heat-based treatments like Endovenous Laser Ablation (EVLA) or Radiofrequency Ablation (RFA) are effective, the glue-based vein closure technique (such as VenaSeal®) is emerging as a top choice for busy individuals who need results without major disruption to their schedules.
Here’s why glue treatment is particularly suited to the demands of professional life.
1. Minimal Downtime
One of the biggest advantages of glue-based closure is how quickly patients can return to work. The procedure is performed under local anaesthesia at a single entry point, takes about 20–30 minutes per vein, and allows patients to walk out of the clinic almost immediately.
Most people can resume desk work, meetings, and even light travel the same day — a huge plus for those who can’t afford extended leave.
2. No Extended Stocking Wear
In India’s warm climate, wearing compression stockings for weeks after treatment can be uncomfortable, especially for those in formal office attire. In many glue-based cases, stockings are not required at all, meaning professionals can dress as usual and avoid the discomfort of medical hosiery during work hours.
3. Single-Session Procedure
Unlike some treatments that require staged sessions or follow-up procedures, glue closure is often completed in one sitting. This means no repeated time off work, no multiple hospital visits, and less disruption to a packed calendar.
4. Needle-Friendly for Comfort
Many professionals delay treatment due to fear of multiple injections. Glue-based treatment needs just one small numbing shot at the entry site, making it a less intimidating choice for those sensitive to needles or concerned about procedural discomfort.
5. Discreet Recovery
There’s no surgical scar, no bandaged leg, and minimal bruising. Professionals can attend meetings, client visits, or conferences without visible signs of a recent procedure. For those in public-facing roles, this discreet recovery is a major confidence booster.
6. Proven, Long-Term Effectiveness
VenaSeal® and similar systems have shown closure rates above 90–95% in long-term studies, meaning most patients enjoy lasting relief without needing repeat interventions. For busy professionals, this means fewer future disruptions and a better return on their investment of time and money.
7. Fits Around a Busy Lifestyle
No hospital admission, no general anaesthesia, and no prolonged rest period — glue closure is designed to fit seamlessly into the lifestyle of someone juggling deadlines, meetings, and travel schedules.
The Bottom Line
Glue-based vein treatment is ideal for working professionals who want an effective, low-disruption solution for varicose veins. With minimal downtime, no long stocking wear, and lasting results, it offers a smart balance of medical success and professional convenience.
At Avis Vascular Centre, our vascular specialists help professionals get back on their feet — and back to business — without missing a beat.