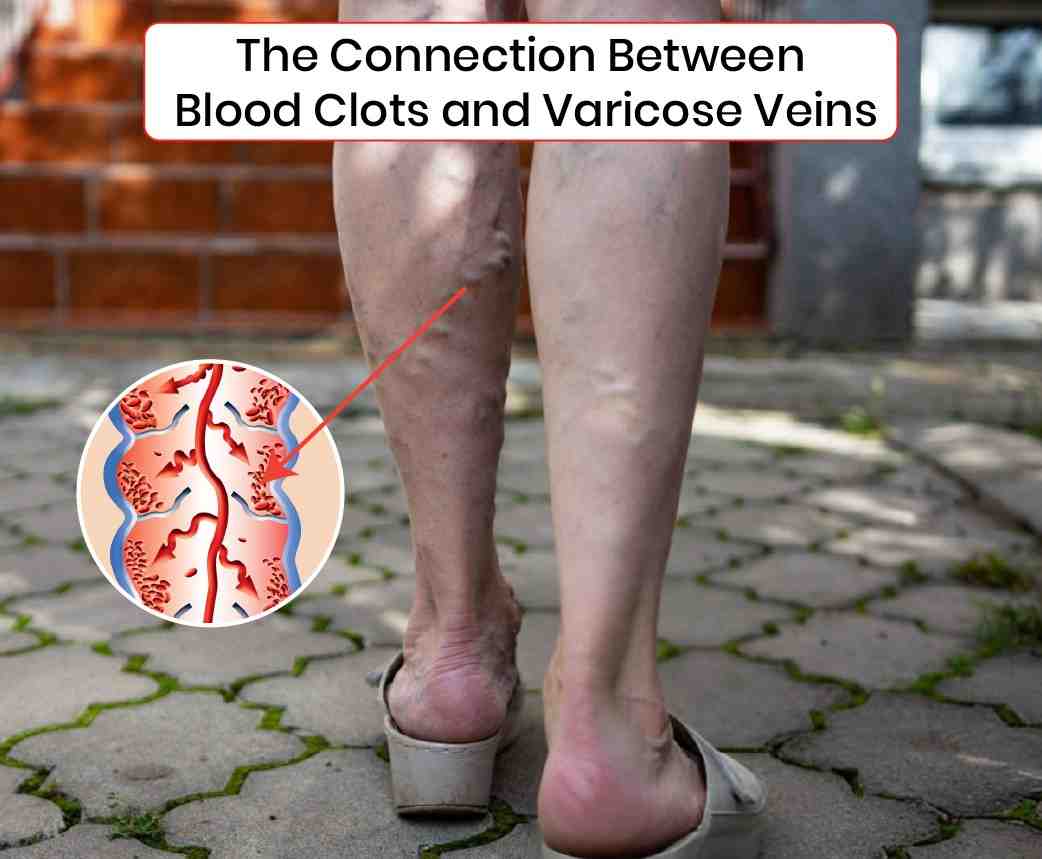
Varicose veins and blood clots are two venous conditions that often coexist and can significantly impact vascular health. While varicose veins are frequently regarded as a cosmetic concern, they may signal underlying venous insufficiency, predisposing individuals to thrombotic events. Understanding the relationship between varicose veins and blood clots is crucial for effective prevention, diagnosis, and treatment.
Varicose Veins: An Overview
Varicose veins are dilated, tortuous superficial veins resulting from venous insufficiency. They commonly appear blue or dark purple and are predominantly found in the lower extremities. The pathophysiology involves valvular incompetence, leading to venous hypertension and venous stasis. This condition is often associated with chronic venous insufficiency (CVI), which further exacerbates venous dysfunction.
Blood Clots: Understanding Thrombosis
Blood clots, or thrombi, form when blood coagulates within the vascular system. While clotting is essential to prevent hemorrhage, pathological thrombosis within veins can be dangerous. Deep vein thrombosis (DVT) refers to clots in deep veins, often in the legs, which can lead to life-threatening complications if embolization occurs, such as pulmonary embolism (PE).
Pathophysiological Connection Between Varicose Veins and Blood Clots
The interplay between varicose veins and thrombus formation is multifaceted:
- Venous Stasis
Venous insufficiency associated with varicose veins results in blood pooling, or stasis, within the venous system. This stasis is a well-known component of Virchow’s triad, which describes the three primary factors contributing to thrombosis: venous stasis, endothelial injury, and hypercoagulability.
- Endothelial Dysfunction and Inflammation
Varicose veins induce chronic inflammation and endothelial dysfunction within the venous wall. These inflammatory processes can activate the coagulation cascade, increasing the risk of thrombus formation.
- Chronic Venous Insufficiency
CVI, commonly accompanying varicose veins, involves prolonged venous hypertension, further promoting thrombotic risk by sustaining an environment conducive to clot formation.
Risk Factors
Several factors predispose individuals to both varicose veins and thrombotic events:
- Age: Advancing age correlates with decreased venous elasticity and valvular competence.
- Genetic Predisposition: A family history of venous disorders increases susceptibility.
- Prolonged Immobility: Extended periods of sitting or standing enhance venous stasis.
- Pregnancy: Hormonal changes and increased venous pressure during pregnancy contribute to venous dilation and stasis.
- Obesity: Excessive body weight exerts additional pressure on the venous system.
- Hormonal Therapy: Hormone replacement therapy and oral contraceptives can elevate thrombotic risk.
Clinical Manifestations
Recognizing the clinical signs of both varicose veins and thrombotic events is imperative for timely intervention:
- Varicose Veins: Visible dilated veins, leg discomfort, heaviness, pruritus, and skin changes such as hyperpigmentation or lipodermatosclerosis.
- Deep Vein Thrombosis: Unilateral leg swelling, erythema, pain or tenderness, and warmth in the affected limb.
Preventive Measures
- Compression Therapy: Graduated compression stockings enhance venous return and reduce stasis.
- Regular Physical Activity: Exercise improves overall vascular health and circulation.
- Leg Elevation: Elevating the legs facilitates venous return and alleviates pressure.
- Weight Management: Maintaining a healthy weight minimizes venous pressure.
Medical and Interventional Treatments
- Sclerotherapy: Injection of a sclerosant into varicose veins induces fibrosis and vein closure.
- Endovenous Laser Therapy (EVLT): Laser energy applied endovenously causes vein ablation.
- Pharmacotherapy: Anticoagulants are prescribed for the prevention and treatment of DVT.
- Surgical Interventions: Vein stripping or ligation may be necessary for severe varicosities.
The connection between varicose veins and blood clots underscores the importance of comprehensive venous health management. Individuals with varicose veins should be vigilant for thrombotic symptoms and seek medical consultation for appropriate evaluation and treatment. Through a combination of lifestyle modifications, pharmacologic interventions, and potentially surgical procedures, the risks associated with varicose veins and blood clots can be effectively managed, ensuring better vascular health and overall well-being.