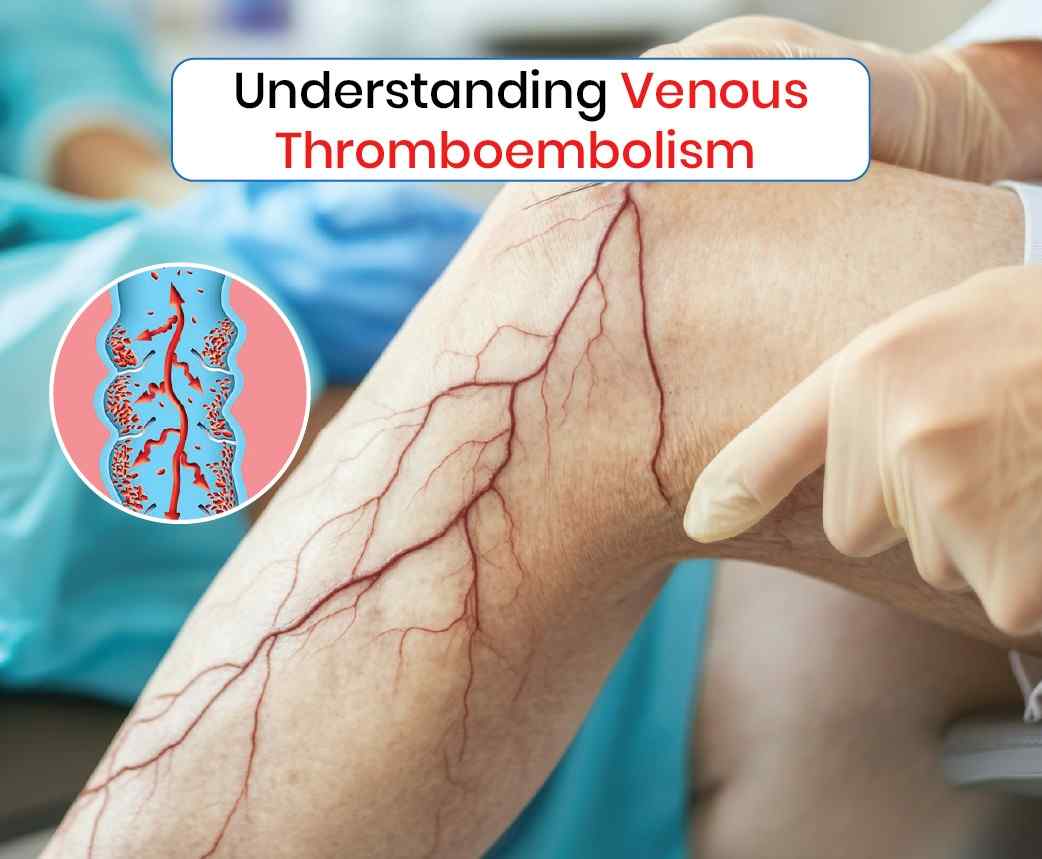
In managing venous thromboembolism (VTE), advanced interventions such as sclerotherapy and ablation have proven to be valuable in treating conditions related to abnormal veins, including chronic venous insufficiency, which can increase the risk of deep vein thrombosis (DVT) and venous clots. While they may not be the primary treatments for acute VTE, these methods are highly effective in addressing underlying venous issues and reducing the risk of future clotting events.
Sclerotherapy: Minimizing the Risk of Clots
What is Sclerotherapy?
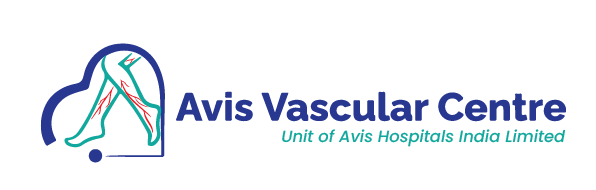
Sclerotherapy is a procedure used to treat varicose veins and spider veins, both of which are associated with poor venous circulation and can contribute to venous insufficiency. During the procedure, a solution is injected into the affected veins, causing them to collapse and eventually be absorbed by the body. The blood is then rerouted through healthier veins, improving overall circulation.
How Sclerotherapy Helps:
- Improved Blood Flow: By closing off damaged veins, sclerotherapy improves circulation in the legs, preventing blood from pooling in the veins. This reduces the risk of developing blood clots, which can form due to stagnant or slow-moving blood.
- Preventing Post-Thrombotic Syndrome: In patients with a history of DVT, sclerotherapy can help treat veins that have been damaged by previous clotting episodes, reducing the chance of developing post-thrombotic syndrome. This condition is characterized by chronic leg pain, swelling, and venous ulcers, which occur due to poor blood flow after a clot has damaged the vein walls.
- Relieving Symptoms of Chronic Venous Insufficiency: Chronic venous insufficiency (CVI) is a condition where veins struggle to return blood to the heart efficiently, often leading to varicose veins and an increased risk of DVT. Sclerotherapy targets the faulty veins responsible for CVI, relieving symptoms and reducing the risk of future clots.
- Minimally Invasive with Quick Recovery: One of the key advantages of sclerotherapy is that it is minimally invasive and requires little downtime, making it an attractive option for patients looking to improve vein health and reduce clotting risk without undergoing major surgery.
Ablation Therapy: A Long-Term Solution for Vein Health
Ablation is a procedure used to treat varicose veins and other vein disorders. It involves using heat (radiofrequency ablation) or laser energy (endovenous laser ablation, or EVLA) to close off problematic veins. Like sclerotherapy, ablation reroutes blood through healthier veins, improving overall circulation and reducing the risk of blood clots.
How Ablation Helps:
- Effective Treatment for Varicose Veins: Varicose veins are a major contributor to chronic venous insufficiency, which can lead to poor circulation and blood pooling in the veins. Ablation effectively treats large varicose veins, reducing the likelihood of clot formation.
- Reducing the Risk of DVT: By sealing off veins that are not functioning properly, ablation improves blood flow and reduces the potential for blood stagnation, a key factor in clot formation. This is particularly important in patients who are at high risk of DVT due to venous insufficiency.
- Preventing Future Venous Complications: Ablation not only improves current circulation issues but also prevents the development of future venous problems, which may otherwise lead to chronic pain, swelling, and an increased risk of clots.
- Minimally Invasive and Long-Lasting: Ablation is a minimally invasive procedure that can be performed in an outpatient setting. Patients typically experience minimal discomfort and can return to normal activities quickly. The long-term success rate of ablation is high, offering a durable solution for venous issues that can lead to clots.
By improving circulation and addressing underlying venous insufficiency, these treatments help reduce the risk of blood clots, prevent future complications, and improve overall vein health. While not directly used to treat acute VTE, they are effective in managing the chronic venous problems that increase the risk of clot formation. These minimally invasive procedures provide long-lasting results and contribute to better long-term outcomes for patients at risk of venous thromboembolism.