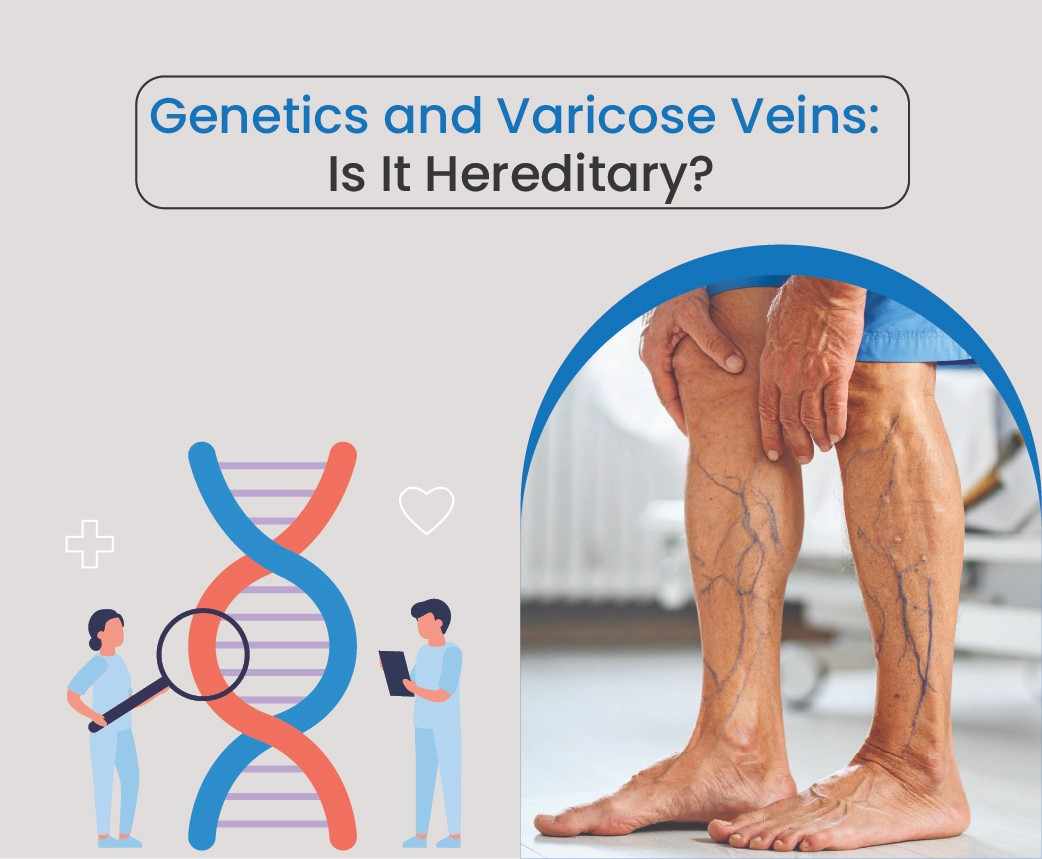
If one or both of your parents had varicose veins, you might wonder whether you’re destined to develop them too. Genetics often influence eye colour, height, or hair texture—but what about vein health? The truth is that heredity plays a significant role in varicose veins, but it’s not the whole story. Let’s explore how family history increases your risk, and what you can do to stay one step ahead.
The Genetic Link Explained
Varicose veins occur when the tiny valves inside veins weaken, allowing blood to flow backward and pool in the legs. This increases pressure, stretching the vein walls and causing them to bulge.
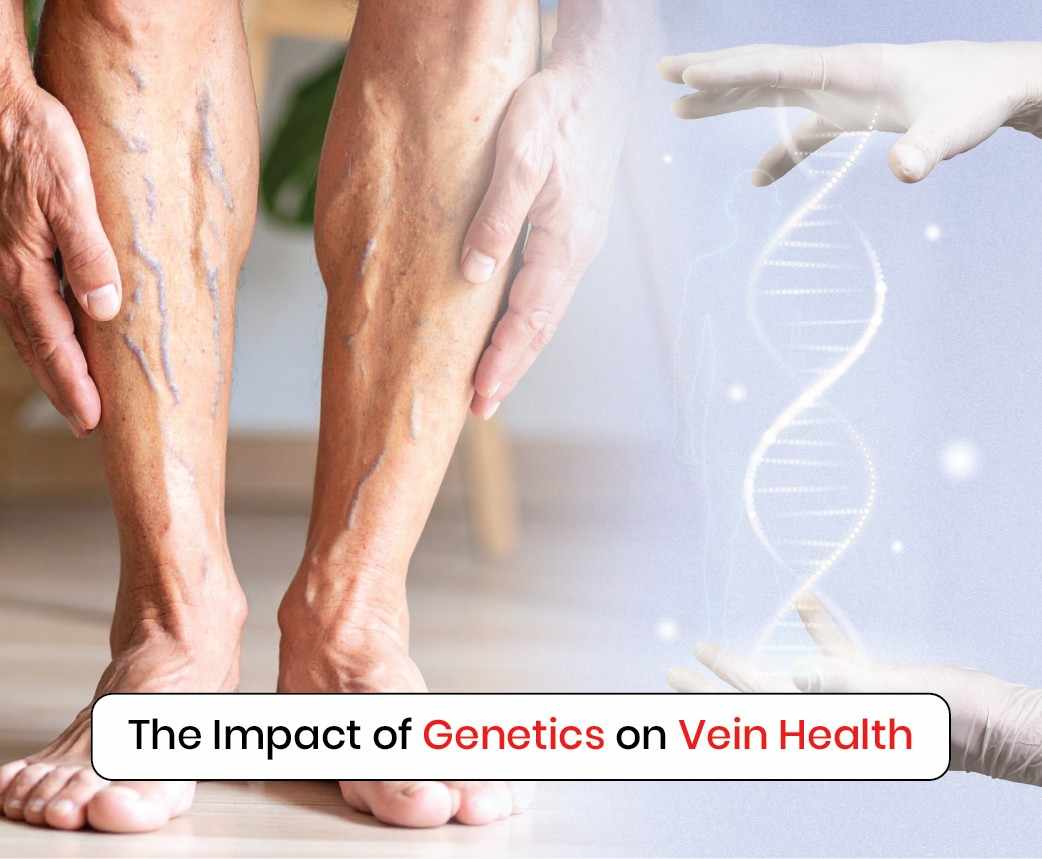
Research shows that genetics are one of the strongest risk factors. If one parent has varicose veins, your risk rises by about 40%. If both parents are affected, that risk can climb as high as 70–80%. The inherited tendency usually involves weaker vein walls or defective valves that make you more vulnerable over time.
Risks and Misconceptions
A common misconception is that if varicose veins “run in the family,” they are inevitable. While genetics increase susceptibility, lifestyle and environmental factors play a huge role. Long hours of sitting or standing, obesity, pregnancy, and lack of exercise can all trigger or worsen varicose veins—even in people without a family history.
Another myth is that only older adults develop hereditary varicose veins. In reality, symptoms can appear as early as your 20s or 30s, especially if you combine genetic risk with poor lifestyle habits. Early warning signs include heaviness, swelling, and aching in the legs after long periods of activity.
Preventive Steps if You Have a Family History
If varicose veins run in your family, proactive care can delay or even prevent their onset. Here are some practical measures:
- Stay active: Walking, cycling, and swimming strengthen calf muscles that support healthy blood flow.
- Maintain a healthy weight: Excess weight puts extra pressure on your veins.
- Avoid prolonged immobility: Take breaks from sitting or standing every 30–60 minutes.
- Elevate your legs whenever possible to encourage circulation.
- Use compression stockings if recommended by a vascular specialist.
Adopting these habits can significantly reduce the burden on your veins, even if you are genetically predisposed.
When to See a Specialist
If you notice visible veins, persistent leg pain, or swelling that doesn’t go away, it’s time to see a vascular surgeon. A duplex ultrasound scan can confirm whether faulty valves are the cause. Today, hereditary varicose veins can be treated effectively with minimally invasive procedures such as endovenous laser treatment (EVLT), radiofrequency ablation (RFA), or foam sclerotherapy. These options target the damaged veins directly, offering quick recovery and long-term relief.
Conclusion
So, is varicose veins hereditary? Yes—genetics increase your risk significantly, but lifestyle factors determine whether and how quickly they develop. The good news is that with preventive care and timely medical treatment, you can manage hereditary risk and protect your vein health.
At Avis Vascular Centre, our team, led by Dr. Rajah V. Koppala, specialises in personalised varicose vein treatments. Whether your condition is hereditary or lifestyle-driven, we provide advanced, minimally invasive solutions for safe and lasting relief. Book a consultation today and take control of your leg health.