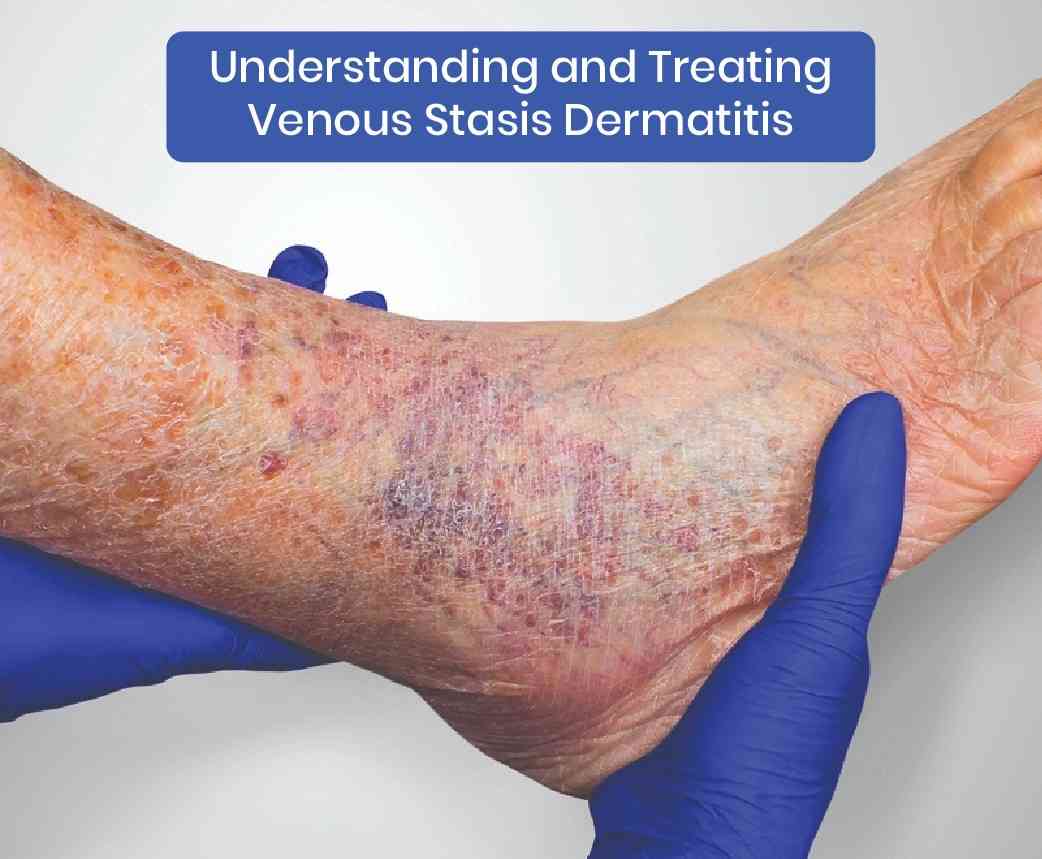
Venous stasis dermatitis, also known as stasis eczema or varicose eczema, is a chronic skin condition that occurs due to poor circulation in the lower extremities. It primarily affects older adults and can lead to significant discomfort and complications if left untreated. In this blog, we will delve into the symptoms, causes, risk factors, and interventional treatment options for venous stasis dermatitis.
Venous stasis dermatitis Symptoms
Venous stasis dermatitis manifests through various signs, which often develop gradually. Common symptoms include:
- Swelling: Particularly around the ankles and lower legs, worsening towards the end of the day.
- Redness and Discoloration: The skin may turn red, brown, or purple due to prolonged poor blood flow.
- Itching and Pain: A persistent itch, along with tenderness or pain, can occur.
- Skin Changes: The skin may become thickened, scaly, or develop a leathery texture.
- Open Sores and Ulcers: Chronic cases can lead to the formation of painful ulcers, often referred to as venous ulcers.
Causes of the condition
The primary cause of venous stasis dermatitis is chronic venous insufficiency (CVI), a condition where the veins in the legs cannot pump blood back to the heart effectively. This inefficiency leads to blood pooling in the lower extremities, increasing pressure within the veins and causing fluid to leak into surrounding tissues. Factors contributing to CVI include:
- Damaged Valves: Vein valves that prevent backflow of blood may become weakened or damaged.
- Varicose Veins: Enlarged veins can disrupt normal blood flow.
- Deep Vein Thrombosis (DVT): Blood clots in deep veins can obstruct blood flow.
Risk Factors
Several factors increase the likelihood of developing venous stasis dermatitis:
- Age: The risk increases with age as veins lose elasticity and valves weaken.
- Gender: Women are more prone to this condition, partly due to hormonal changes.
- Family History: A family history of vein problems can predispose individuals.
- Lifestyle: Prolonged standing or sitting, lack of exercise, and obesity can contribute.
- Medical History: Previous leg injuries, surgeries, or conditions like congestive heart failure and hypertension.
What are the available Treatment Options?
Treating venous stasis dermatitis involves addressing both the skin condition and the underlying venous insufficiency. A multifaceted approach typically includes:
Lifestyle Modifications
- Compression Therapy: Wearing compression stockings helps reduce swelling and improves blood flow.
- Exercise: Regular physical activity promotes circulation and vein health.
- Leg Elevation: Elevating the legs above heart level can alleviate swelling.
Medical Treatments
- Topical Medications: Corticosteroids and moisturizers can reduce inflammation and soothe the skin.
- Antibiotics: For cases with secondary bacterial infection, antibiotics may be prescribed.
- Wound Care: Proper care of any ulcers or open sores is crucial to prevent infection and promote healing.
Surgical and Minimally Invasive Procedures
- Sclerotherapy: A procedure where a solution is injected into varicose veins, causing them to collapse and be reabsorbed by the body.
- Laser Therapy: Laser treatments can close off affected veins.
- Vein Stripping and Ligation: Surgical removal or tying off of problematic veins in severe cases.
Early diagnosis and intervention are key to preventing complications and improving quality of life. If you experience symptoms of venous stasis dermatitis, consult a healthcare professional to develop a comprehensive treatment plan tailored to your needs. Call our expert Vein doctors at Avis vascular center today and begin your journey towards healthy veins and a better life.