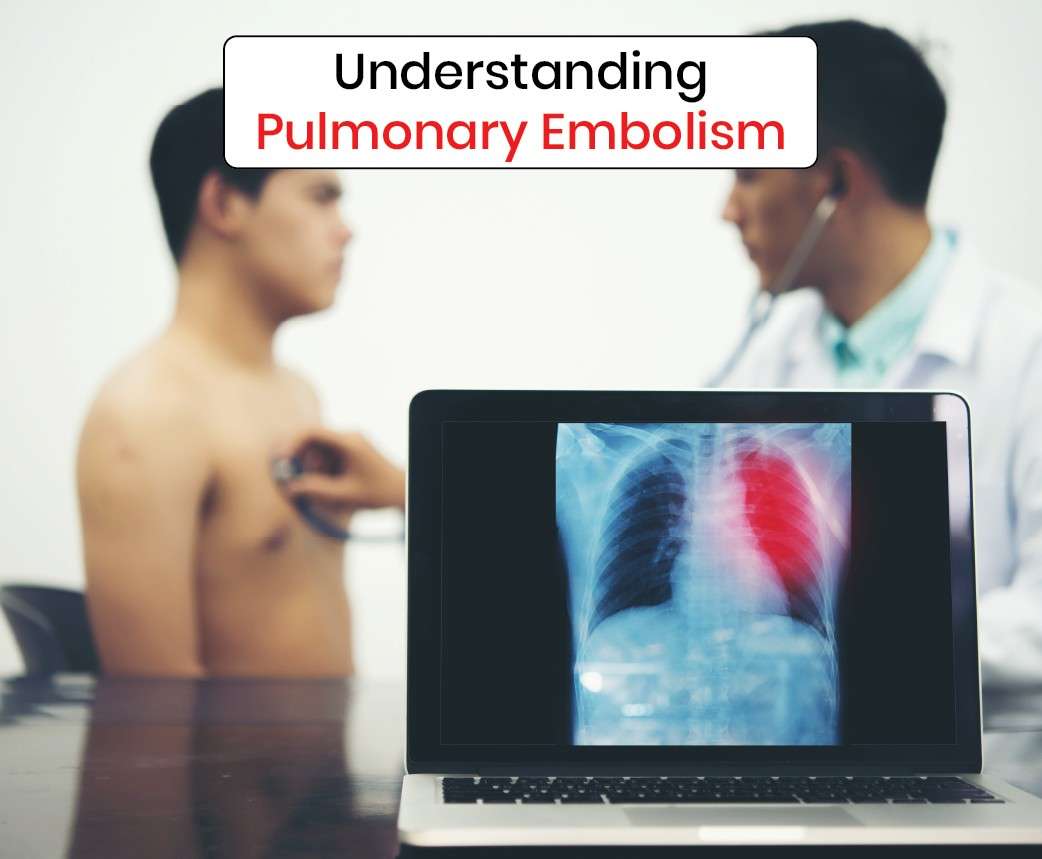
Pulmonary embolism (PE) is a potentially life-threatening condition characterized by the sudden blockage of one or more arteries in the lungs. This blockage typically occurs when a blood clot, usually originating from the deep veins of the legs (a condition known as deep vein thrombosis or DVT), travels through the bloodstream and lodges in the pulmonary arteries. Understanding the implications of pulmonary embolism on life expectancy and the factors influencing recovery is crucial for patients and healthcare providers alike.
The Mechanism of Pulmonary Embolism:
Pulmonary embolism occurs when a blood clot, or a fragment of a clot, breaks loose from its site of origin and travels through the veins to the lungs. Factors that increase the risk of blood clot formation include prolonged immobility, surgery, trauma, obesity, pregnancy, and certain medical conditions such as cancer and inherited clotting disorders. Once in the pulmonary circulation, the clot can obstruct blood flow to the lungs, leading to potentially severe consequences.
Symptoms and Diagnosis:
The symptoms of pulmonary embolism can vary widely depending on the size and location of the clot. Common signs and symptoms include sudden onset of chest pain, shortness of breath, rapid heartbeat, coughing (sometimes with bloody sputum), and fainting. However, some individuals may experience no symptoms at all, especially if the clot is small. Diagnosis typically involves a combination of medical history, physical examination, imaging tests (such as CT pulmonary angiography), and blood tests (such as D-dimer assay).
Life Expectancy After Pulmonary Embolism:
The prognosis and life expectancy following a pulmonary embolism depend on several factors, including the size of the clot, the extent of lung involvement, the presence of underlying medical conditions, and the timeliness and effectiveness of treatment. Prompt recognition and appropriate management are crucial in improving outcomes and reducing the risk of complications.
Immediate Treatment and Management:
Immediate treatment for pulmonary embolism aims to stabilize the patient and prevent further clot formation. This often involves the administration of anticoagulant medications (such as heparin or low-molecular-weight heparin) to prevent the existing clot from growing and new clots from forming. In some cases, thrombolytic therapy may be considered to dissolve the clot more rapidly, particularly in patients with massive or life-threatening PE. Additional supportive measures, such as supplemental oxygen and pain management, may also be necessary.
Long-Term Management and Recovery:
Central to the management of pulmonary embolism is the recognition of its close association with deep vein thrombosis (DVT), emphasizing the paramount importance of vein treatment. Addressing underlying venous insufficiencies and clots in the lower extremities significantly reduces the risk of thrombus formation, thus preventing potential embolic events like PE.
By implementing strategies to improve venous circulation and prevent clot formation through interventions such as compression therapy, anticoagulation, and minimally invasive procedures like Sclerotherapy, and ablation techniques, healthcare providers can effectively disrupt the vicious cycle of clot formation.
Moreover, early detection and treatment of venous insufficiency not only mitigate the risk of PE but also alleviate symptoms, enhance quality of life, and contribute to long-term vascular health. Therefore, prioritizing vein treatment plays a pivotal role not only in managing acute pulmonary embolism but also in preventing its recurrence and optimizing patient outcomes.