Blood clots and Peripheral Artery Disease (PAD) are serious conditions that affect the circulatory system, often leading to life-threatening complications if untreated. Both conditions can impede blood flow, causing pain, discomfort, and more severe health problems. Understanding their symptoms, risks, and treatment options is key to managing these conditions.
What are Blood Clots
A blood clot forms when blood changes from a liquid to a gel-like state, often as a response to injury. However, when clots form inside veins or arteries without injury, they can cause significant problems. These clots can block blood flow, leading to conditions like deep vein thrombosis (DVT) or pulmonary embolism (PE).
DVT occurs when a clot forms in the deep veins, typically in the legs, causing swelling, pain, and redness.
PE happens if a DVT travels to the lungs, blocking blood flow and causing chest pain, difficulty breathing, or even death.
Common risk factors for blood clots include prolonged immobility, surgery, smoking, obesity, and underlying health issues like heart disease.
Peripheral Artery Disease (PAD)
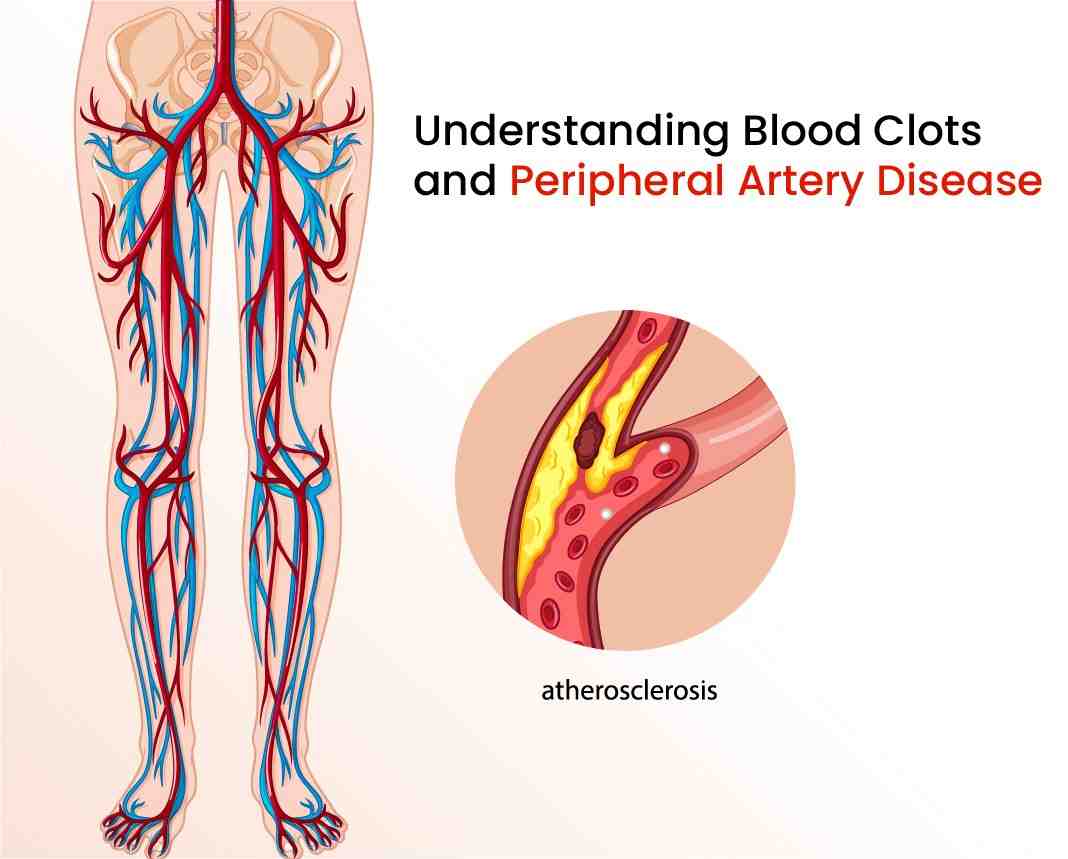
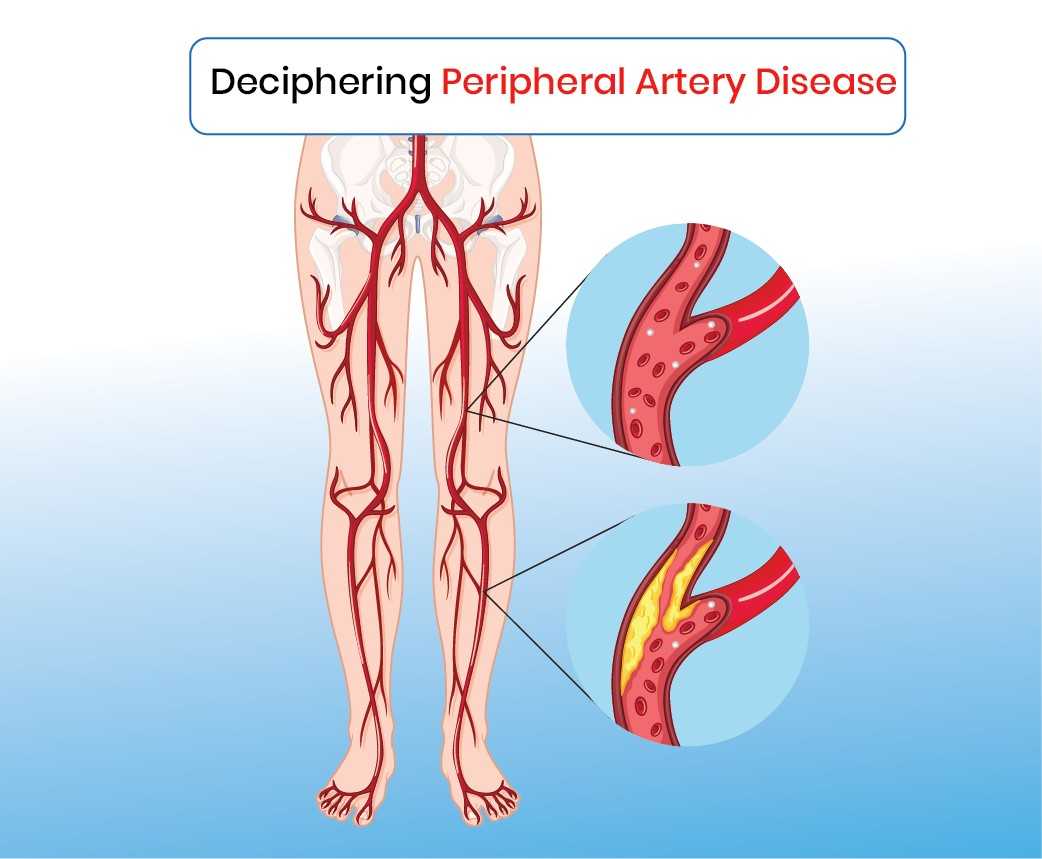
PAD occurs when narrowed arteries reduce blood flow to the limbs, typically the legs. This condition is caused by atherosclerosis, where fatty deposits block arteries. PAD often leads to symptoms such as:
Claudication (leg pain while walking): Pain or cramping in the calf, thigh, or hip.
Cold or numb feet and toes: Poor blood circulation makes the extremities feel unusually cold.
Ulcers or sores on the legs or feet that heal slowly or not at all.
PAD is more common in people with diabetes, high blood pressure, and high cholesterol. Early symptoms may be mild, making the condition hard to detect, but untreated PAD can lead to heart attacks, strokes, and amputations.
Connection Between Blood Clots and PAD
While PAD and blood clots are different conditions, they are linked through poor circulation. People with PAD have a higher risk of developing blood clots because narrowed arteries slow blood flow, increasing the likelihood of clotting. Both conditions share risk factors like smoking, obesity, and high cholesterol.
Treatment Options at Avis Vascular Center
At Avis Vascular Center, a leading healthcare facility specializing in vascular care, patients receive expert diagnosis and treatment for blood clots and PAD. The center offers interventional treatments that are less invasive and highly effective.
For blood clots, anticoagulants (blood thinners) are commonly prescribed to prevent clot formation, while severe cases may require thrombolytics to dissolve clots. Avis Vascular Center also offers catheter-directed thrombolysis, a cutting-edge procedure that directly delivers medication to the clot.
Preventing blood clots and PAD involves managing risk factors through a healthy lifestyle—regular exercise, a balanced diet, and avoiding smoking are critical. Early detection and expert care at facilities like Avis Vascular Center can prevent complications and ensure better outcomes.
Blood clots and PAD are serious, but manageable with the right treatment. Early diagnosis and the latest interventional therapies offered by Avis Vascular Center can significantly improve patients’ quality of life and prevent severe complications.