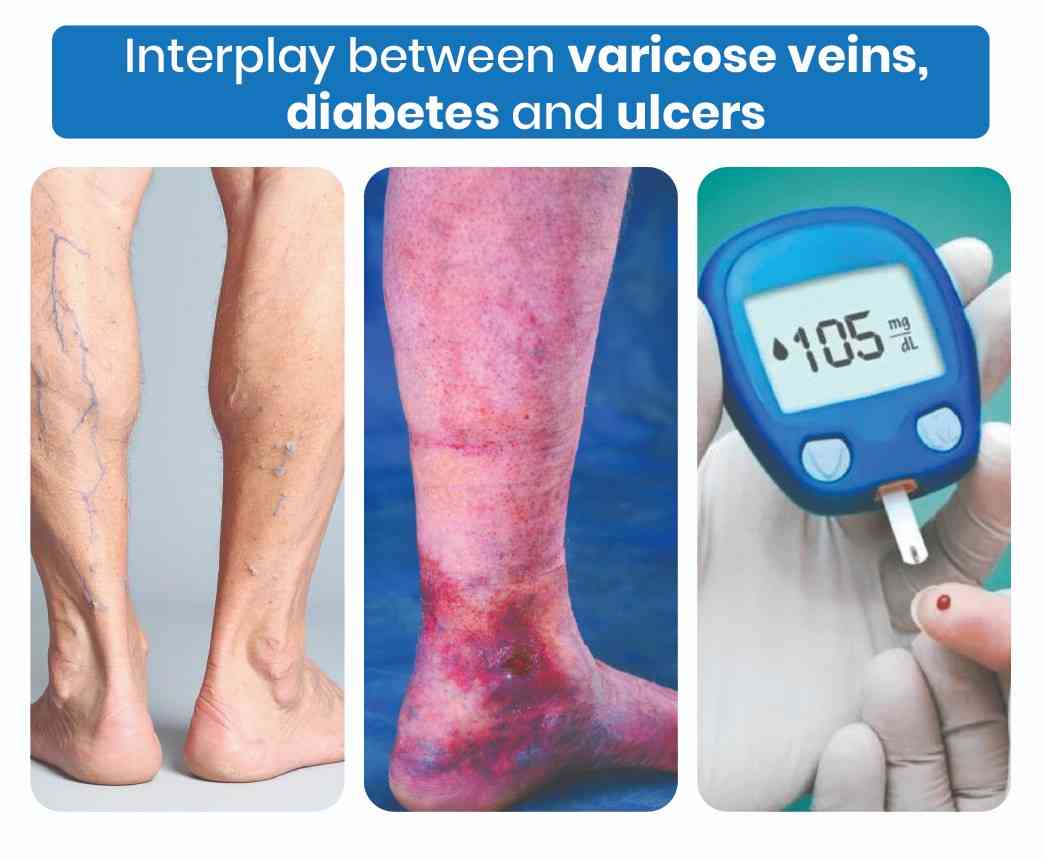
Varicose veins, often regarded as a cosmetic issue, can profoundly impact individuals, particularly those with concurrent medical conditions like diabetes. The presence of leg ulcers that resist healing, coupled with leg swelling and discomfort, may signify complications stemming from varicose veins. This intricate relationship warrants a deeper exploration into the mechanisms by which varicose veins exacerbate ulcers and how diabetes intertwines with these vascular concerns.
Varicose Veins and Leg Ulcers: Mechanisms of Aggravation
Varicose veins arise from weakened or damaged valves within the veins, leading to venous insufficiency and impaired blood flow. Over time, this venous dysfunction culminates in elevated pressure within the veins, resulting in various manifestations, including:
Chronic Venous Insufficiency (CVI): The compromised venous circulation associated with varicose veins contributes to CVI, characterized by inadequate blood return to the heart. CVI fosters a hostile environment conducive to ulcer formation, particularly in the lower extremities.
Circulatory Disturbances: Varicose veins disrupt the circulation within the skin, compromising wound healing mechanisms. Prolonged venous hypertension and capillary leakage aggravate tissue damage, rendering ulcers refractory to conventional treatment approaches.
Inflammatory Cascade: Venous stasis induced by varicose veins triggers an inflammatory response, perpetuating tissue damage and impeding the reparative processes crucial for ulcer resolution. Chronic inflammation fosters a protracted ulcerative state, further complicating management strategies.
The Diabetic Factor: Unraveling the Connection
Individuals with diabetes face an augmented risk of vascular complications due to microvascular and macrovascular pathology inherent to the disease. The interplay between diabetes and varicose veins underscores several key points:
- Vascular Problems Get Worse with Diabetes: Diabetes makes the issues caused by varicose veins worse. It increases the chances of having ulcers on your legs and makes it harder for wounds to heal. Diabetes damages the tiny blood vessels and nerves in your legs, making the problem even worse.
- Immune System Doesn’t Work Right: Diabetes messes up your immune system, which affects how your body fights off infections. This makes it harder for wounds to heal properly. When combined with varicose veins, it creates more inflammation and makes healing even more difficult.
- Nerve Damage Makes Things Tough: Diabetes can damage the nerves in your legs, leading to problems with feeling and moving your legs properly. This makes it harder to get blood flowing well in your legs, which can worsen the issues caused by varicose veins. Managing these nerve problems alongside varicose veins can be challenging and may require different specialists to help.
Strategic Interventions: Addressing Varicose Veins and Diabetes Complications
Effective management of varicose veins and associated ulcers in diabetic individuals necessitates a comprehensive therapeutic approach tailored to address the intricate interplay between vascular dysfunction and metabolic derangements. Key interventions include:
- Compression Therapy: Utilizing graduated compression stockings to mitigate venous hypertension and facilitate blood return, thereby ameliorating ulceration and enhancing wound healing.
- Endovascular Interventions: Employing minimally invasive procedures like sclerotherapy and endovenous ablation to target varicose veins and mitigate venous insufficiency, alleviating ulcerative burden and fostering ulcer resolution.
- Diabetes Optimization: Rigorous glycemic control and meticulous foot care are paramount in mitigating diabetic complications and fostering ulcer healing. Close collaboration between vascular specialists and endocrinologists is imperative to optimize diabetes management and mitigate vascular sequelae.
Varicose veins represent more than just a cosmetic concern, posing a significant risk for the development and exacerbation of leg ulcers, particularly in individuals with diabetes. Understanding the intricate mechanisms by which varicose veins potentiate ulcerative burden and intertwine with diabetic complications is paramount in formulating effective therapeutic strategies.
By addressing varicose veins and optimizing diabetes management through a multidisciplinary approach, healthcare providers can mitigate ulcerative morbidity and foster optimal vascular health in affected individuals.