Vein problems, particularly those involving the deep veins of the legs, are a significant risk factor for the development of blood clots. These clots can cause a range of serious health complications if they travel through the bloodstream or obstruct vital circulation pathways. For medical professionals, understanding the relationship between vein disorders and the complications of blood clots is crucial for preventing severe outcomes and managing patient care effectively.
Vein Problems and Their Role in Blood Clot Formation
Veins are responsible for returning deoxygenated blood back to the heart. When these veins are compromised, it can lead to poor circulation and an increased risk of blood clots. Several common vein problems are particularly associated with the formation of blood clots:
- Chronic Venous Insufficiency (CVI): CVI occurs when the veins in the legs do not efficiently return blood to the heart due to damaged vein valves. This causes blood to pool in the legs, leading to swelling, pain, and skin changes. The stagnant blood flow can increase the risk of clot formation, particularly in the deep veins, resulting in deep vein thrombosis (DVT).
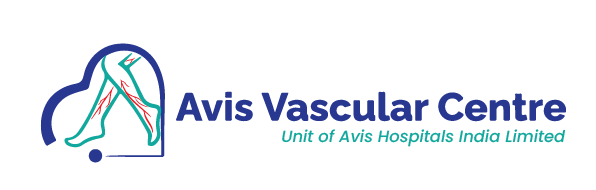
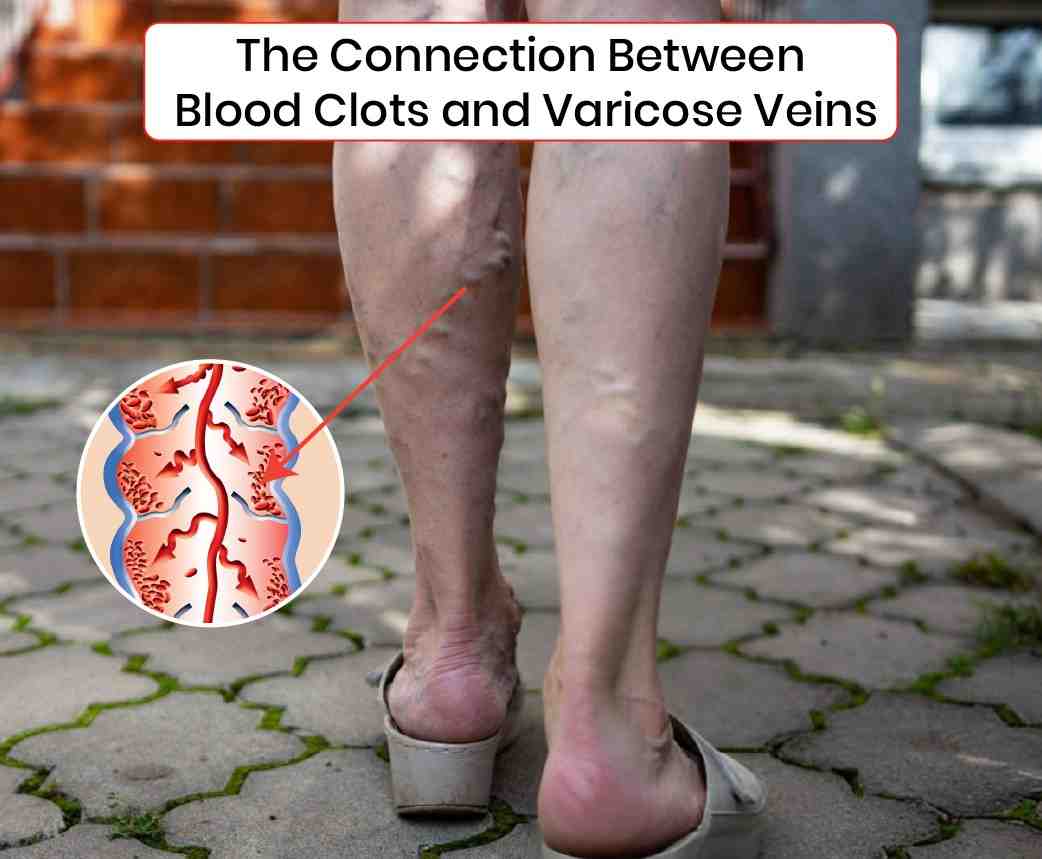
- Varicose Veins: These are enlarged, twisted veins that are often visible just under the surface of the skin. While they are typically a cosmetic concern, they can also indicate underlying vein problems such as CVI. The sluggish blood flow in varicose veins creates a conducive environment for clotting. Although less common, varicose veins can contribute to superficial vein thrombosis, which, while less dangerous than DVT, can still be painful and cause further complications.
- Deep Vein Thrombosis (DVT): This condition involves the formation of a clot in the deep veins, usually in the legs. DVT is particularly dangerous because if part of the clot breaks free, it can travel through the bloodstream and lodge in the lungs, causing a pulmonary embolism (PE). This is a life-threatening complication that can lead to severe respiratory distress and even death.
Complications Arising from Vein-Related Blood Clots
When blood clots form due to vein problems, they can lead to a range of serious complications. Here are some of the most concerning:
- Pulmonary Embolism (PE): When a clot formed in the deep veins (DVT) travels to the lungs, it can cause a pulmonary embolism. PE blocks blood flow in the lungs, which can lead to sudden shortness of breath, chest pain, and even death if not treated immediately. The connection between DVT and PE underscores the importance of early detection and treatment of vein problems.
- Post-Thrombotic Syndrome (PTS): This condition can develop in up to 50% of patients who have had a DVT. PTS results from long-term damage to the vein valves caused by the clot, leading to chronic pain, swelling, and in severe cases, ulcers. PTS significantly impacts a patient’s quality of life and highlights the long-term consequences of untreated vein issues.
- Chronic Venous Insufficiency (CVI): Following a DVT, patients are at higher risk of developing chronic venous insufficiency. The clot can damage the vein valves permanently, leading to persistent symptoms such as leg swelling, varicose veins, skin changes, and venous ulcers. This condition further increases the risk of future clot formation and requires ongoing management.
Prevention and Management of Vein-Related Blood Clot Complications
Preventing complications from blood clots due to vein problems involves several strategies:
- Compression Therapy: Wearing compression stockings can help improve blood flow in the legs and reduce the risk of clot formation in patients with chronic venous insufficiency or varicose veins. Compression therapy is often recommended for patients post-DVT to prevent PTS.
- Anticoagulation Therapy: Patients with a history of DVT or those at high risk of clot formation may be prescribed anticoagulants to reduce the chance of clotting. However, this requires careful monitoring to balance the risk of bleeding complications.
- Lifestyle Modifications: Regular exercise, weight management, and elevating the legs can help improve venous circulation and reduce the risk of clots. Patients are also advised to avoid prolonged periods of immobility, which can exacerbate vein problems and increase clot risk.
Understanding the relationship between vein disorders and blood clot complications is essential for healthcare providers to prevent severe outcomes and provide effective management strategies for patients. Early diagnosis and proactive treatment are key to mitigating the risks associated with these conditions and ensuring better patient outcomes.